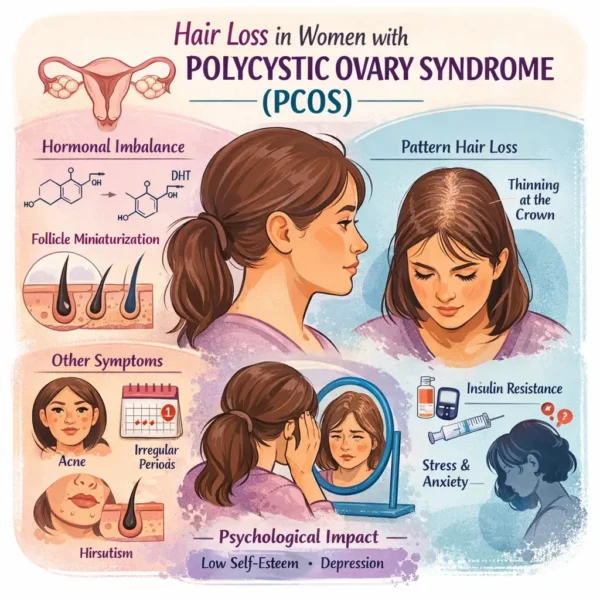
Polycystic ovary syndrome (PCOS) is a common endocrine disorder affecting women of reproductive age, with an estimated prevalence of approximately 4–7% (using the original National Institutes of Health diagnostic criteria) and higher rates when broader criteria are applied. PCOS is a heterogeneous condition characterized by varying combinations of ovulatory dysfunction, hyperandrogenism (hyperandrogenemia means having excess androgens hormones like testosterone in the body), polycystic ovarian morphology, and metabolic abnormalities. Among its cutaneous manifestations, hair loss – which most commonly presents as androgenetic alopecia or female pattern hair loss (FPHL) – represents one of the most psychologically distressing features for affected women.
Clinical patterns of hair loss in PCOS: Hair loss in women with PCOS most frequently manifests as androgenetic alopecia (AGA), also referred to as female pattern hair loss (FPHL). This is a non-scarring alopecia characterized by progressive miniaturization of terminal hair follicles into finer, shorter vellus-like hairs. The process reflects a shortening of the anagen (growth) phase and an increase in the proportion of hairs in telogen, resulting in reduced hair density and volume over time.
The clinical pattern of androgen-related hair loss differs markedly between women and men. While men typically develop bitemporal hairline recession and vertex balding on the top of the scalp, women with AGA usually exhibit diffuse thinning over the crown and mid-scalp with preservation of the frontal hairline. This distinction is clinically important and helps differentiate AGA from other causes of diffuse hair loss, including telogen effluvium and diffuse alopecia areata.
Prevalence of androgenetic alopecia in PCOS: Despite AGA being widely recognized as a manifestation of hyperandrogenism, its prevalence in women with PCOS has historically been under-studied outside of dermatologic literature. Reported prevalence rates vary widely, ranging from approximately 3% to 35% depending on population characteristics, diagnostic criteria, and study design.
The largest and most systematic evaluation to date examined over 250 women diagnosed with PCOS according to the Rotterdam criteria and found a prevalence of androgenetic alopecia in the group of approximately 22%. This figure aligns closely with pooled estimates from recent systematic reviews and meta-analyses, which report a prevalence of roughly 23% among women with PCOS. Notably, prevalence appears higher in cohorts of patients diagnosed using methods that confirm presence of hyperandrogenism, supporting the notion that androgen excess contributes to follicular vulnerability.
Conversely, studies evaluating women presenting primarily with patterned hair loss features have demonstrated a strikingly high prevalence of polycystic ovarian morphology. Ultrasound-based studies have reported polycystic ovaries in up to two-thirds of women with androgenetic alopecia, even in the absence of overt biochemical hyperandrogenemia (as tested for using blood samples). These findings support a bi-directional association between PCOS and female pattern hair loss, with each condition serving as a potential clinical marker for the other.
Androgens, follicles, and local hormone metabolism: The role of androgen hormones in the pathogenesis of AGA is well established in men, where dihydrotestosterone (DHT), derived from testosterone via the enzyme 5-alpha reductase, acts on androgen receptors in genetically susceptible hair follicles to drive miniaturization. In women, the relationship is more complicated. Many women with AGA – including those with PCOS – have androgen levels in their blood that are within laboratory reference ranges, and correlations between serum androgen concentrations and hair loss severity are inconsistent.
Several studies have failed to demonstrate significant differences in total testosterone, free testosterone, or biochemical hyperandrogenemia between women with PCOS – in patients both with and without AGA. However, clinical markers of androgen excess such as acne and hirsutism are consistently more prevalent in women with PCOS-associated hair loss, suggesting that systemic hormone measurements may not fully reflect follicular androgen exposure.
Local androgen metabolism within the hair follicle is increasingly recognized as a key determinant of hair loss. Investigations of ovarian tissue in PCOS have demonstrated markedly elevated 5-alpha reductase activity, resulting in increased local conversion of testosterone to DHT. Although ovarian tissue differs from scalp follicles, these findings suggest there may be a broader disease model in which hair follicle tissue-specific androgen metabolism, rather than circulating hormone levels alone, contributes to the PCOS manifestations of AGA and hirsutism.
Sex hormone–binding globulin (SHBG) may further modulate androgen bioavailability. Several studies have observed lower SHBG concentrations in women with AGA, including those with PCOS; this might increase free androgen exposure at the follicular level. Importantly, low SHBG has also been linked to metabolic risk in PCOS, raising the possibility that hair loss may cluster with other adverse conditions even in the absence of overt hyperandrogenemia.
Metabolic and endocrine modifiers: PCOS is strongly associated with insulin resistance, obesity, and metabolic syndrome, yet the relationship between these factors and hair loss remains unclear. In younger cohorts of women with PCOS, studies have generally failed to demonstrate differences in insulin resistance indices, body mass index, waist-to-hip ratio, or glucose tolerance between those with and without androgenetic alopecia.
This contrasts with findings from older population-based studies in which female pattern hair loss was quite strongly associated with insulin resistance and metabolic abnormalities. Age may be a critical modifier, with cumulative metabolic stress contributing to follicular miniaturization over time. Alternatively, metabolic factors may act indirectly by lowering SHBG or altering adrenal and ovarian steroidogenesis.
Emerging evidence also implicates hypothalamic–pituitary–adrenal (HPA) axis dysregulation in PCOS. Studies measuring hair cortisol (a marker of long-term cortisol exposure) have demonstrated significantly elevated levels in women with PCOS compared with controls. In those with high hair cortisol concentrations, cortisol levels correlate with androgen indices, inflammatory markers, insulin resistance, and adiposity. These findings raise the possibility that chronic stress physiology may amplify endocrine and metabolic disturbances relevant to hair follicle function, although direct links to scalp hair loss remain to be established.
Psychological impact of hair loss in PCOS: Hair loss represents a particularly distressing manifestation of PCOS, often affecting young women during formative years of identity and self-image. PCOS itself is associated with increased rates of anxiety, depression, and negative body image, and androgenetic alopecia independently carries a substantial psychological burden.
Women with PCOS and AGA consistently report greater concern regarding hair loss than those without alopecia. Interestingly, formal measures of depression do not always differ significantly between these groups, suggesting that the psychological impact of PCOS may be substantial regardless of hair status. Nonetheless, mean depression scores in PCOS cohorts frequently exceed screening thresholds. Some research studies emphasize the importance of routine mental health assessment for patients with PCOS and hair loss.
Clinical implications and future directions: The relationship between PCOS and female pattern hair loss is complex and multifactorial. Hair loss in PCOS cannot be reliably predicted by serum androgen levels alone and may reflect local androgen metabolism, follicular sensitivity, SHBG availability, stress physiology, and genetic susceptibility. The presence of androgenetic alopecia in women – particularly when accompanied by acne, hirsutism, or menstrual irregularity – should prompt evaluation for PCOS and associated metabolic risks.
Conversely, clinicians caring for women with PCOS should proactively assess scalp hair changes, as hair loss may be underreported despite its known impact on patients’ quality of life. Current evidence supports a bidirectional association between PCOS and female pattern hair loss, with overlapping pathophysiologic mechanisms and therapeutic considerations.
Future research priorities include longitudinal studies to clarify causality, investigations of follicle-level androgen signaling in women, and integration of emerging biomarkers such as hair cortisol and hair follicle/skin tissue-specific steroid metabolism. Improved understanding of these mechanisms may ultimately enable more targeted, individualized treatment strategies for hair loss in women with PCOS.
Summary: Overall, hair loss in PCOS represents a visible and distressing manifestation of a systemic endocrine disorder. Recognizing its prevalence, heterogeneity, and underlying biology is essential for holistic patient care and for advancing research at the intersection of dermatology, endocrinology, and women’s health.
Bibliography
11711645 {11711645:296N3YZC},{11711645:3HT9N77K},{11711645:JCL5MIRB},{11711645:YYIJD3F9},{11711645:Q4SW5YZW},{11711645:9IHCZSE6},{11711645:L4UN69CC},{11711645:WMVTF9AY},{11711645:DNBPC4YG},{11711645:AV9Z3A8C},{11711645:X7I3UU8I},{11711645:7WUU93CJ},{11711645:SJGGBFWJ} 1 vancouver 50 date asc 2032 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%227WUU93CJ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Miyazaki%20et%20al.%22%2C%22parsedDate%22%3A%221978-09%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BMiyazaki%20M%2C%20Takayasu%20S%2C%20Karakawa%20T%2C%20Aono%20T%2C%20Kurachi%20K%2C%20Matsumoto%20K.%20Activity%20of%20testosterone%205alpha-reductase%20in%20the%20hair%20follicles%20of%20women%20with%20polycystic%20ovaries.%20J%20Endocrinol.%201978%20Sept%3B78%283%29%3A445%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Activity%20of%20testosterone%205alpha-reductase%20in%20the%20hair%20follicles%20of%20women%20with%20polycystic%20ovaries%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Miyazaki%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22Takayasu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Karakawa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Aono%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%22%2C%22lastName%22%3A%22Kurachi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%22%2C%22lastName%22%3A%22Matsumoto%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221978-09%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1677%5C%2Fjoe.0.0780445%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220022-0795%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A19%3A08Z%22%7D%7D%2C%7B%22key%22%3A%22WMVTF9AY%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Futterweit%20et%20al.%22%2C%22parsedDate%22%3A%221988-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFutterweit%20W%2C%20Dunaif%20A%2C%20Yeh%20HC%2C%20Kingsley%20P.%20The%20prevalence%20of%20hyperandrogenism%20in%20109%20consecutive%20female%20patients%20with%20diffuse%20alopecia.%20J%20Am%20Acad%20Dermatol.%201988%20Nov%3B19%285%20Pt%201%29%3A831%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20prevalence%20of%20hyperandrogenism%20in%20109%20consecutive%20female%20patients%20with%20diffuse%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22W.%22%2C%22lastName%22%3A%22Futterweit%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Dunaif%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22H.%20C.%22%2C%22lastName%22%3A%22Yeh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Kingsley%22%7D%5D%2C%22abstractNote%22%3A%22Endocrine%20dysfunction%20was%20studied%20in%20109%20consecutive%20female%20patients%20with%20moderate%20to%20severe%20alopecia%2C%20mostly%20of%20a%20diffuse%20pattern.%20The%20study%20included%20an%20evaluation%20of%20associated%20hirsutism%20and%5C%2For%20menstrual%20dysfunction%2C%20plasma%20hormonal%20measurements%2C%20and%20ultrasonography%20of%20the%20ovaries.%20A%20control%20group%20of%2024%20ovulatory%2C%20nonhirsute%2C%20nonalopecia%20individuals%20was%20also%20studied.%20Of%20the%20109%20patients%2C%2070%20%2864.2%25%29%20had%20no%20clinical%20evidence%20of%20hirsutism%20or%20menstrual%20dysfunction.%20Two%20of%2044%20patients%20tested%20with%20cosyntropin%20%28Cortrosyn%29%20had%2021-hydroxylase%20deficiency%2C%20whereas%20two%20other%20patients%20had%20hyperprolactinemia%20caused%20by%20pituitary%20tumors.%20Hyperandrogenism%20was%20defined%20as%20an%20increase%20in%20any%20of%20the%20plasma%20androgens%20%28testosterone%2C%20non-sex%20hormone-binding%20globulin%20bound%20testosterone%2C%20dehydroepiandrosterone%20sulfate%2C%20androstenedione%2C%20or%20dihydrotestosterone%29%20and%20was%20noted%20in%2042%20of%20the%20109%20patients%20studied%20%2838.5%25%29.%20Of%20these%2042%20patients%2C%2011%20were%20ovulatory%20with%20no%20evidence%20of%20clinical%20hirsutism%2C%2013%20were%20ovulatory%20and%20hirsute%2C%20and%2018%20had%20oligomenorrhea%20or%20amenorrhea%20with%20or%20without%20hirsutism%20with%20confirmatory%20evidence%20of%20polycystic%20ovarian%20disease.%20Patients%20with%20diffuse%20alopecia%20may%20demonstrate%20hyperandrogenism%2C%20even%20in%20the%20absence%20of%20hirsutism%2C%20oligomenorrhea%2C%20or%20amenorrhea.%20The%20most%20common%20endocrine%20disorder%20in%20this%20series%20of%20patients%20with%20diffuse%20alopecia%20was%20polycystic%20ovarian%20disease.%22%2C%22date%22%3A%221988-11%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fs0190-9622%2888%2970241-8%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220190-9622%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A38%3A41Z%22%7D%7D%2C%7B%22key%22%3A%22L4UN69CC%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Jakimiuk%20et%20al.%22%2C%22parsedDate%22%3A%221999-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BJakimiuk%20AJ%2C%20Weitsman%20SR%2C%20Magoffin%20DA.%205alpha-reductase%20activity%20in%20women%20with%20polycystic%20ovary%20syndrome.%20J%20Clin%20Endocrinol%20Metab.%201999%20July%3B84%287%29%3A2414%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%225alpha-reductase%20activity%20in%20women%20with%20polycystic%20ovary%20syndrome%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20J.%22%2C%22lastName%22%3A%22Jakimiuk%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%20R.%22%2C%22lastName%22%3A%22Weitsman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%20A.%22%2C%22lastName%22%3A%22Magoffin%22%7D%5D%2C%22abstractNote%22%3A%22The%20recent%20demonstration%20of%20high%20concentrations%20of%205alpha-androstane-3%2C17-dione%20in%20the%20follicular%20fluid%20of%20polycystic%20ovaries%20suggests%20a%20potential%20role%20for%205alpha-reduced%20androgens%20in%20the%20etiology%20of%20polycystic%20ovary%20syndrome%20%28PCOS%29.%20The%20purpose%20of%20the%20present%20study%20was%20to%20determine%20whether%20there%20is%20increased%205alpha-reductase%20activity%20or%20messenger%20ribonucleic%20acid%20%28mRNA%29%20expression%20in%20polycystic%20ovaries.%205alpha-Reductase%201%20and%205alpha-reductase%202%20mRNAs%20were%20measured%20in%20thecal%20%28TC%29%20and%20granulosa%20%28GC%29%20cells%20from%20individual%20follicles%20of%2018%20women%20with%20PCOS%20and%2026%20regularly%20cycling%20control%20women.%20Both%205alpha-reductase%201%20and%202%20mRNA%20expression%20was%20higher%20in%20GC%20than%20in%20TC%2C%20and%205alpha-reductase%202%20mRNA%20levels%20were%20approximately%203-fold%20higher%20than%205alpha-reductase%201%20mRNA.%205alpha-Reductase%201%20and%202%20mRNA%20expression%20were%20similar%20in%20GC%20from%20PCOS%20and%20control%20women%2C%20but%205alpha-reductase%20mRNA%20was%20decreased%20in%20TC%20from%20PCOS%20follicles.%20In%20control%20women%2C%205alpha-reductase%202%20mRNA%20was%20highest%20in%20GC%20from%203-%20to%205-mm%20follicles%20and%20decreased%20to%20undetectable%20levels%20in%20GC%20from%207-mm%20follicles.%20A%20similar%20pattern%20of%20expression%20was%20present%20in%20GC%20from%20PCOS%20follicles%2C%20but%20detectable%20levels%20of%205alpha-reductase%202%20mRNA%20were%20present%20in%20GC%20from%207-mm%20follicles.%205alpha-Reductase%20activity%20was%20measured%20in%20whole%20follicles%20by%20measuring%20the%20conversion%20of%20radiolabeled%20testosterone%20to%20dihydrotestosterone.%20Kinetic%20analysis%20of%20total%205alpha-reductase%20activity%20at%20physiological%20pH%20revealed%20a%20Km%20of%201.46%20micromol%5C%2FL%20and%20a%20maximal%20velocity%20of%200.31%20nmol%5C%2Fmin%20x%20mg%20protein%2C%20indicating%20predominantly%20type%201%20activity.%20The%20total%205alpha-reductase%20activity%20was%20approximately%204-fold%20higher%20in%20PCOS%20follicles%20than%20in%20control%20follicles.%20These%20data%20demonstrate%20elevated%205alpha-reductase%20activity%20in%20polycystic%20ovaries%20and%20support%20the%20hypothesis%20that%205alpha-reduced%20androgens%20may%20play%20a%20role%20in%20the%20pathogenesis%20of%20PCOS.%22%2C%22date%22%3A%221999-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1210%5C%2Fjcem.84.7.5863%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220021-972X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A44%3A58Z%22%7D%7D%2C%7B%22key%22%3A%22Q4SW5YZW%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Birch%20et%20al.%22%2C%22parsedDate%22%3A%222001-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BBirch%20MP%2C%20Messenger%20JF%2C%20Messenger%20AG.%20Hair%20density%2C%20hair%20diameter%20and%20the%20prevalence%20of%20female%20pattern%20hair%20loss.%20Br%20J%20Dermatol.%202001%20Feb%3B144%282%29%3A297%26%23x2013%3B304.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hair%20density%2C%20hair%20diameter%20and%20the%20prevalence%20of%20female%20pattern%20hair%20loss%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20P.%22%2C%22lastName%22%3A%22Birch%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%20F.%22%2C%22lastName%22%3A%22Messenger%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20G.%22%2C%22lastName%22%3A%22Messenger%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Female%20pattern%20hair%20loss%20is%20common%20but%20estimates%20of%20its%20prevalence%20have%20varied%20widely.%20The%20relationships%20between%20the%20clinical%20diagnosis%20of%20female%20pattern%20hair%20loss%20and%20objective%20measurements%20of%20hair%20density%20and%20hair%20diameter%20have%20not%20previously%20been%20evaluated.%5CnOBJECTIVES%3A%20To%20determine%20the%20prevalence%20of%20female%20pattern%20hair%20loss%20and%20to%20relate%20the%20clinical%20findings%20to%20hair%20density%20and%20hair%20diameter.%5CnMETHODS%3A%20We%20examined%20377%20women%2C%20aged%2018--99%20years%2C%20who%20presented%20to%20a%20general%20dermatology%20clinic%20with%20complaints%20unrelated%20to%20hair%20growth%20%28the%20unselected%20sample%29.%20A%20second%20group%20of%2047%20women%20referred%20with%20typical%20female%20pattern%20hair%20loss%20was%20included%20in%20analyses%20of%20the%20relationships%20between%20hair%20density%2C%20hair%20diameter%20and%20the%20clinical%20diagnosis.%20Hair%20density%20was%20measured%20using%20a%20photographic%20method.%20In%20each%20subject%20the%20major%20and%20minor%20axis%20diameters%20were%20measured%20in%20a%20random%20sample%20of%2050%20hairs.%5CnRESULTS%3A%20Six%20per%20cent%20of%20women%20aged%20under%2050%20years%20were%20diagnosed%20as%20having%20female%20pattern%20hair%20loss%2C%20increasing%20to%2038%25%20in%20subjects%20aged%2070%20years%20and%20over.%20The%20mean%20%2B%5C%2F-%20SEM%20hair%20density%20was%20293%20%2B%5C%2F-%2061.3%20hairs%20cm%28-2%29%20at%20age%2035%20years%2C%20falling%20to%20211%20%2B%5C%2F-%2055.1%20hairs%20cm%28-2%29%20at%20age%2070%20years.%20Hair%20density%20showed%20a%20normal%20distribution%20in%20the%20unselected%20sample.%20Most%20women%20classified%20as%20having%20female%20pattern%20hair%20loss%20had%20hair%20densities%20within%20the%20lower%20half%20of%20the%20normal%20distribution.%20The%20perception%20of%20hair%20loss%20was%20determined%20mainly%20by%20low%20hair%20density%20%28ANOVA%20P%20%26lt%3B%200.001%29%2C%20but%20there%20was%20overlap%20in%20hair%20density%20between%20women%20classified%20as%20having%20Ludwig%20I%20hair%20loss%20and%20the%20no%20hair%20loss%20group%2C%20which%20was%20partly%20accounted%20for%20by%20differences%20in%20mean%20hair%20diameter%20%28ANOVA%20P%20%26lt%3B%200.001%29.%20Low%20hair%20density%20was%20associated%20with%20fewer%20hairs%20of%20all%20diameters.%5CnCONCLUSIONS%3A%20Hair%20density%20in%20women%20is%20distributed%20as%20a%20normal%20variable%2C%20indicating%20that%20it%20is%20determined%20as%20a%20multifactorial%20trait.%20Women%20with%20female%20pattern%20hair%20loss%20have%20a%20hair%20density%20which%20falls%20below%20the%20mean%20but%20lies%20within%20the%20spectrum%20of%20the%20normal%20distribution%2C%20although%20other%20factors%2C%20including%20hair%20diameter%2C%20may%20affect%20the%20subjective%20impression%20of%20hair%20loss.%20The%20hair%20diameter%20data%20suggest%20that%20low%20hair%20density%20is%20not%20due%20to%20progressive%20diminution%20in%20hair%20follicle%20size%20and%20that%20follicular%20miniaturization%20may%20occur%20within%20the%20space%20of%20a%20single%20hair%20cycle.%22%2C%22date%22%3A%222001-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1046%5C%2Fj.1365-2133.2001.04018.x%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220007-0963%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A50%3A12Z%22%7D%7D%2C%7B%22key%22%3A%22SJGGBFWJ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Cela%20et%20al.%22%2C%22parsedDate%22%3A%222003-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCela%20E%2C%20Robertson%20C%2C%20Rush%20K%2C%20Kousta%20E%2C%20White%20DM%2C%20Wilson%20H%2C%20et%20al.%20Prevalence%20of%20polycystic%20ovaries%20in%20women%20with%20androgenic%20alopecia.%20Eur%20J%20Endocrinol.%202003%20Nov%3B149%285%29%3A439%26%23x2013%3B42.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Prevalence%20of%20polycystic%20ovaries%20in%20women%20with%20androgenic%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ester%22%2C%22lastName%22%3A%22Cela%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Carole%22%2C%22lastName%22%3A%22Robertson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Karen%22%2C%22lastName%22%3A%22Rush%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eleni%22%2C%22lastName%22%3A%22Kousta%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Davinia%20M.%22%2C%22lastName%22%3A%22White%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Helen%22%2C%22lastName%22%3A%22Wilson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Glenn%22%2C%22lastName%22%3A%22Lyons%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Philip%22%2C%22lastName%22%3A%22Kingsley%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mark%20I.%22%2C%22lastName%22%3A%22McCarthy%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stephen%22%2C%22lastName%22%3A%22Franks%22%7D%5D%2C%22abstractNote%22%3A%22OBJECTIVE%3A%20Although%20androgenic%20alopecia%20is%20recognised%20to%20be%20a%20symptom%20of%20polycystic%20ovary%20syndrome%20%28PCOS%29%2C%20it%20is%20not%20known%20whether%20polycystic%20ovaries%20%28PCO%29%20and%20associated%20endocrine%20abnormalities%20are%20present%20in%20patients%20who%20present%20with%20alopecia%20as%20a%20primary%20complaint.%20We%20therefore%20set%20out%20to%20determine%20the%20strength%20of%20the%20association%20between%20androgenic%20alopecia%20and%20PCO.%20We%20examined%20the%20prevalence%20of%20ultrasound-based%20polycystic%20ovarian%20morphology%20and%20associated%20clinical%20and%20biochemical%20features%20in%20a%20large%20multiethnic%20group%20of%20women%20whose%20presenting%20complaint%20was%20of%20alopecia%2C%20and%20in%20a%20control%20group.%5CnSUBJECTS%20AND%20METHODS%3A%20We%20studied%2089%20women%20of%20mixed%20ethnic%20origin%20with%20androgenic%20alopecia%20and%20compared%20them%20to%2073%20control%20women.%20A%20detailed%20history%20was%20taken%2C%20anthropometry%20was%20performed%20and%20assessment%20of%20body-hair%20distribution%20was%20made.%20The%20presence%20of%20PCO%20was%20established%20by%20pelvic%20ultrasound%20scan.%20Serum%20gonadotrophins%2C%20testosterone%2C%20androstenedione%2C%20dihydrotestosterone%20and%20sex%20hormone%20binding%20globulin%20concentrations%20were%20measured.%5CnRESULTS%3A%20Women%20with%20alopecia%20had%20a%20higher%20prevalence%20of%20PCO%20and%20hirsutism%20than%20the%20control%20population%20%28PCO%3A%2067%25%20vs%2027%25%2C%20P%26lt%3B0.00001%3B%20hirsutism%3A%2021%25%20vs%204%25%2C%20P%3D0.003%29.%20Women%20with%20alopecia%20%28with%20or%20without%20PCO%29%20had%20higher%20testosterone%2C%20androstenedione%20and%20free%20androgen%20index%20than%20controls%2C%20even%20though%20few%20had%20frankly%20abnormal%20androgens.%5CnCONCLUSIONS%3A%20These%20findings%20confirm%20an%20association%20between%20androgenic%20alopecia%20and%20PCO%2C%20and%20other%20symptoms%20of%20hyperandrogenaemia.%20Thus%20most%20women%20who%20present%20with%20androgenic%20alopecia%20as%20their%20primary%20complaint%20also%20have%20PCO%20and%20have%20indices%20of%20abnormal%20androgen%20production.%20Since%20PCO%20is%20a%20well%20known%20risk%20factor%20for%20development%20of%20type%202%20diabetes%2C%20this%20association%20has%20important%20implications%20for%20long-term%20management.%22%2C%22date%22%3A%222003-11%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1530%5C%2Feje.0.1490439%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220804-4643%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A16%3A44Z%22%7D%7D%2C%7B%22key%22%3A%22AV9Z3A8C%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Azziz%20et%20al.%22%2C%22parsedDate%22%3A%222004-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAzziz%20R%2C%20Sanchez%20LA%2C%20Knochenhauer%20ES%2C%20Moran%20C%2C%20Lazenby%20J%2C%20Stephens%20KC%2C%20et%20al.%20Androgen%20excess%20in%20women%3A%20experience%20with%20over%201000%20consecutive%20patients.%20J%20Clin%20Endocrinol%20Metab.%202004%20Feb%3B89%282%29%3A453%26%23x2013%3B62.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Androgen%20excess%20in%20women%3A%20experience%20with%20over%201000%20consecutive%20patients%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%22%2C%22lastName%22%3A%22Azziz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%20A.%22%2C%22lastName%22%3A%22Sanchez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E.%20S.%22%2C%22lastName%22%3A%22Knochenhauer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Moran%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Lazenby%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%20C.%22%2C%22lastName%22%3A%22Stephens%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%22%2C%22lastName%22%3A%22Taylor%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%20R.%22%2C%22lastName%22%3A%22Boots%22%7D%5D%2C%22abstractNote%22%3A%22The%20objective%20of%20the%20present%20study%20was%20to%20estimate%20the%20prevalence%20of%20the%20different%20pathological%20conditions%20causing%20clinically%20evident%20androgen%20excess%20and%20to%20document%20the%20degree%20of%20long-term%20success%20of%20suppressive%20and%5C%2For%20antiandrogen%20hormonal%20therapy%20in%20a%20large%20consecutive%20population%20of%20patients.%20All%20patients%20presenting%20for%20evaluation%20of%20symptoms%20potentially%20related%20to%20androgen%20excess%20between%20October%201987%20and%20June%202002%20were%20evaluated%2C%20and%20the%20data%20were%20maintained%20prospectively%20in%20a%20computerized%20database.%20For%20the%20assessment%20of%20therapeutic%20response%2C%20a%20retrospective%20review%20of%20the%20medical%20chart%20was%20performed%2C%20after%20the%20exclusion%20of%20those%20patients%20seeking%20fertility%20therapy%20only%2C%20or%20with%20inadequate%20follow-up%20or%20poor%20compliance.%20A%20total%20of%201281%20consecutive%20patients%20were%20seen%20during%20the%20study%20period.%20Excluded%20from%20analysis%20were%20408%20patients%20in%20whom%20we%20were%20unable%20to%20evaluate%20hormonal%20status%2C%20determine%20ovulatory%20status%2C%20or%20find%20any%20evidence%20of%20androgen%20excess.%20In%20the%20remaining%20population%20of%20873%20patients%2C%20the%20unbiased%20prevalence%20of%20androgen-secreting%20neoplasms%20was%200.2%25%2C%2021-hydroxylase-deficient%20classic%20adrenal%20hyperplasia%20%28CAH%29%20was%200.6%25%2C%2021-hydroxylase-deficient%20nonclassic%20adrenal%20hyperplasia%20%28NCAH%29%20was%201.6%25%2C%20hyperandrogenic%20insulin-resistant%20acanthosis%20nigricans%20%28HAIRAN%29%20syndrome%20was%203.1%25%2C%20idiopathic%20hirsutism%20was%204.7%25%2C%20and%20polycystic%20ovary%20syndrome%20%28PCOS%29%20was%2082.0%25.%20Fifty-nine%20%286.75%25%29%20patients%20had%20elevated%20androgen%20levels%20and%20hirsutism%20but%20normal%20ovulation.%20A%20total%20of%20257%20patients%20were%20included%20in%20the%20assessment%20of%20the%20response%20to%20hormonal%20therapy.%20The%20mean%20duration%20of%20follow-up%20was%2033.5%20months%20%28range%2C%206-155%29.%20Hirsutism%20improved%20in%2086%25%2C%20menstrual%20dysfunction%20in%2080%25%2C%20acne%20in%2081%25%2C%20and%20hair%20loss%20in%2033%25%20of%20patients.%20The%20major%20side%20effects%20noted%20were%20irregular%20vaginal%20bleeding%20%2816.1%25%29%2C%20nausea%20%2813.0%25%29%2C%20and%20headaches%20%2812.6%25%29%3B%20only%2036.6%25%20of%20patients%20never%20complained%20of%20side%20effects.%20In%20this%20large%20study%20of%20consecutive%20patients%20presenting%20with%20clinically%20evident%20androgen%20excess%2C%20specific%20identifiable%20disorders%20%28NCAH%2C%20CAH%2C%20HAIRAN%20syndrome%2C%20and%20androgen-secreting%20neoplasms%29%20were%20observed%20in%20approximately%207%25%20of%20subjects%2C%20whereas%20functional%20androgen%20excess%2C%20principally%20PCOS%2C%20was%20observed%20in%20the%20remainder.%20Hirsutism%2C%20menstrual%20dysfunction%2C%20or%20acne%2C%20but%20not%20alopecia%2C%20improved%20in%20the%20majority%20of%20patients%20treated%20with%20a%20combination%20suppressive%20therapy%3B%20although%20more%20than%2060%25%20experienced%20side%20effects.%22%2C%22date%22%3A%222004-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1210%5C%2Fjc.2003-031122%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220021-972X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A37%3A13Z%22%7D%7D%2C%7B%22key%22%3A%22DNBPC4YG%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Carmina%20et%20al.%22%2C%22parsedDate%22%3A%222006-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCarmina%20E%2C%20Rosato%20F%2C%20Jann%26%23xEC%3B%20A%2C%20Rizzo%20M%2C%20Longo%20RA.%20Extensive%20clinical%20experience%3A%20relative%20prevalence%20of%20different%20androgen%20excess%20disorders%20in%20950%20women%20referred%20because%20of%20clinical%20hyperandrogenism.%20J%20Clin%20Endocrinol%20Metab.%202006%20Jan%3B91%281%29%3A2%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Extensive%20clinical%20experience%3A%20relative%20prevalence%20of%20different%20androgen%20excess%20disorders%20in%20950%20women%20referred%20because%20of%20clinical%20hyperandrogenism%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E.%22%2C%22lastName%22%3A%22Carmina%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22F.%22%2C%22lastName%22%3A%22Rosato%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Jann%5Cu00ec%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Rizzo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%20A.%22%2C%22lastName%22%3A%22Longo%22%7D%5D%2C%22abstractNote%22%3A%22CONTEXT%3A%20We%20undertook%20this%20study%20to%20estimate%20the%20prevalence%20of%20the%20various%20androgen%20excess%20disorders%20using%20the%20new%20criteria%20suggested%20for%20the%20diagnosis%20of%20polycystic%20ovary%20syndrome%20%28PCOS%29.%5CnSETTING%3A%20The%20study%20was%20performed%20at%20two%20endocrine%20departments%20at%20the%20University%20of%20Palermo%20%28Palermo%2C%20Italy%29.%5CnPATIENTS%3A%20The%20records%20of%20all%20patients%20referred%20between%201980%20and%202004%20for%20evaluation%20of%20clinical%20hyperandrogenism%20were%20reevaluated.%20All%20past%20diagnoses%20were%20reviewed%20using%20the%20actual%20diagnostic%20criteria.%20To%20be%20included%20in%20this%20study%2C%20the%20records%20of%20the%20patients%20had%20to%20present%20the%20following%20available%20data%3A%20clinical%20evaluation%20of%20hyperandrogenism%2C%20body%20weight%20and%20height%2C%20testosterone%20%28T%29%2C%20free%20T%2C%20dehydroepiandrosterone%20sulfate%2C%2017-hydroxyprogesterone%2C%20progesterone%2C%20and%20pelvic%20sonography.%20A%20total%20of%201226%20consecutive%20patients%20were%20seen%20during%20the%20study%20period%2C%20but%20only%20the%20scores%20of%20950%20patients%20satisfied%20all%20criteria%20and%20were%20reassessed%20for%20the%20diagnosis.%5CnRESULTS%3A%20The%20prevalence%20of%20androgen%20excess%20disorders%20was%3A%20PCOS%2C%2072.1%25%20%28classic%20anovulatory%20patients%2C%2056.6%25%3B%20mild%20ovulatory%20patients%2C%2015.5%25%29%2C%20idiopathic%20hyperandrogenism%2C%2015.8%25%3B%20idiopathic%20hirsutism%2C%207.6%25%3B%2021-hydroxylase-deficient%20nonclassic%20adrenal%20hyperplasia%2C%204.3%25%3B%20and%20androgen-secreting%20tumors%2C%200.2%25.%20Compared%20with%20other%20androgen%20excess%20disorders%2C%20patients%20with%20PCOS%20had%20increased%20body%20weight%20whereas%20nonclassic%20adrenal%20hyperplasia%20patients%20were%20younger%20and%20more%20hirsute%20and%20had%20higher%20serum%20levels%20of%20T%2C%20free%20T%2C%20and%2017-hydroxyprogesterone.%5CnCONCLUSIONS%3A%20Classic%20PCOS%20is%20the%20most%20common%20androgen%20excess%20disorder.%20However%2C%20mild%20androgen%20excess%20disorders%20%28ovulatory%20PCOS%20and%20idiopathic%20hyperandrogenism%29%20are%20also%20common%20and%2C%20in%20an%20endocrine%20setting%2C%20include%20about%2030%25%20of%20patients%20with%20clinical%20hyperandrogenism.%22%2C%22date%22%3A%222006-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1210%5C%2Fjc.2005-1457%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220021-972X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A38%3A25Z%22%7D%7D%2C%7B%22key%22%3A%22X7I3UU8I%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Quinn%20et%20al.%22%2C%22parsedDate%22%3A%222014-04%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BQuinn%20M%2C%20Shinkai%20K%2C%20Pasch%20L%2C%20Kuzmich%20L%2C%20Cedars%20M%2C%20Huddleston%20H.%20Prevalence%20of%20androgenic%20alopecia%20in%20patients%20with%20polycystic%20ovary%20syndrome%20and%20characterization%20of%20associated%20clinical%20and%20biochemical%20features.%20Fertil%20Steril.%202014%20Apr%3B101%284%29%3A1129%26%23x2013%3B34.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Prevalence%20of%20androgenic%20alopecia%20in%20patients%20with%20polycystic%20ovary%20syndrome%20and%20characterization%20of%20associated%20clinical%20and%20biochemical%20features%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Molly%22%2C%22lastName%22%3A%22Quinn%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kanade%22%2C%22lastName%22%3A%22Shinkai%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lauri%22%2C%22lastName%22%3A%22Pasch%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lili%22%2C%22lastName%22%3A%22Kuzmich%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marcelle%22%2C%22lastName%22%3A%22Cedars%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Heather%22%2C%22lastName%22%3A%22Huddleston%22%7D%5D%2C%22abstractNote%22%3A%22OBJECTIVE%3A%20To%20describe%20the%20prevalence%20of%20androgenic%20alopecia%20%28AGA%29%20in%20patients%20with%20polycystic%20ovary%20syndrome%20%28PCOS%29%20and%20to%20characterize%20associated%20clinical%20and%20biochemical%20features.%5CnDESIGN%3A%20Cross-sectional%20study.%5CnSETTING%3A%20Multidisciplinary%20PCOS%20clinic%20at%20a%20tertiary%20academic%20center.%5CnPATIENT%28S%29%3A%20A%20total%20of%20254%20women%20with%20PCOS%20according%20to%20the%20Rotterdam%20criteria%20were%20systematically%20examined%20from%202007%20to%202012%20by%20a%20reproductive%20endocrinologist%2C%20a%20dermatologist%2C%20and%20a%20psychologist.%5CnINTERVENTION%28S%29%3A%20Comprehensive%20dermatologic%20exams%2C%20ultrasonic%20imaging%2C%20serum%20testing%2C%20and%20Beck%20Depression%20Inventory%20Fast%20Screen%20%28BDI-FS%29.%5CnMAIN%20OUTCOME%20MEASURES%3A%20Presence%20of%20AGA%2C%20acne%2C%20hirsutism%2C%20biochemical%20hyperandrogenemia%2C%20metabolic%20dysfunction%2C%20and%20clinical%20depression.%5CnRESULT%28S%29%3A%20Fifty-six%20of%20254%20patients%20with%20PCOS%20%2822.0%25%29%20had%20AGA.%20Subjects%20with%20PCOS%20and%20AGA%20were%20more%20likely%20to%20have%20acne%20or%20hirsutism%20than%20those%20without%20AGA%20%2896.3%25%20vs.%2070.6%25%29.%20Subjects%20with%20AGA%20were%20more%20likely%20to%20report%20concern%20with%20hair%20loss%20%2870.4%25%20vs.%2037.7%25%29%3B%20however%2C%20their%20BDI-FS%20scores%20were%20no%20different%20from%20subjects%20without%20AGA.%20There%20were%20no%20differences%20between%20subjects%20with%20and%20without%20AGA%20in%20biochemical%20hyperandrogenism%20or%20metabolic%20parameters.%5CnCONCLUSION%28S%29%3A%20AGA%20is%20prevalent%20in%2022%25%20of%20subjects%20meeting%20diagnostic%20criteria%20for%20PCOS.%20AGA%20is%20associated%20with%20other%20manifestations%20of%20clinical%20hyperandrogenism%2C%20but%20not%20with%20greater%20risk%20of%20biochemical%20hyperandrogenemia%20or%20metabolic%20dysfunction%20than%20with%20PCOS%20alone.%22%2C%22date%22%3A%222014-04%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.fertnstert.2014.01.003%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221556-5653%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A19%3A55Z%22%7D%7D%2C%7B%22key%22%3A%22296N3YZC%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Prasad%20et%20al.%22%2C%22parsedDate%22%3A%222020-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BPrasad%20S%2C%20De%20Souza%20B%2C%20Burns%20LJ%2C%20Lippincott%20M%2C%20Senna%20MM.%20Polycystic%20ovary%20syndrome%20in%20patients%20with%20hair%20thinning.%20J%20Am%20Acad%20Dermatol.%202020%20July%3B83%281%29%3A260%26%23x2013%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Polycystic%20ovary%20syndrome%20in%20patients%20with%20hair%20thinning%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sonya%22%2C%22lastName%22%3A%22Prasad%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Brianna%22%2C%22lastName%22%3A%22De%20Souza%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Laura%20J.%22%2C%22lastName%22%3A%22Burns%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Margaret%22%2C%22lastName%22%3A%22Lippincott%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maryanne%20M.%22%2C%22lastName%22%3A%22Senna%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222020-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2020.01.075%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A58%3A59Z%22%7D%7D%2C%7B%22key%22%3A%223HT9N77K%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Gonzalez%20et%20al.%22%2C%22parsedDate%22%3A%222022-06-20%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BGonzalez%20D%2C%20Maidana%20P%2C%20Ibar%20C%2C%20Jamardo%20J%2C%20Jacobsen%20D%2C%20Fritzler%20A%2C%20et%20al.%20Hair%20cortisol%20in%20polycystic%20ovary%20syndrome.%20Sci%20Rep.%202022%20June%2020%3B12%281%29%3A10309.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hair%20cortisol%20in%20polycystic%20ovary%20syndrome%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Gonzalez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Maidana%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Ibar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Jamardo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Jacobsen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Fritzler%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22F.%22%2C%22lastName%22%3A%22Fortuna%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G.%22%2C%22lastName%22%3A%22Fernandez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E.%22%2C%22lastName%22%3A%22Lamas-Majek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22Mallea-Gil%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Ballarino%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Onetto%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Lopez%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Viviana%22%2C%22lastName%22%3A%22Mesch%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%22%2C%22lastName%22%3A%22Fabre%22%7D%5D%2C%22abstractNote%22%3A%22The%20aim%20of%20the%20study%20was%20to%20evaluate%20adrenal%20axis%20hyperactivation%20measuring%20hair%20cortisol%20levels%2C%20and%20its%20influence%20on%20the%20relationship%20among%20metabolic%20parameters%2C%20inflammation%20markers%20and%20androgens%20in%20adult%20women%20with%20PCOS.%2044%20women%20%2818-34%5Cu00a0years%29%20with%20PCOS%20diagnosis%20and%20a%20control%20group%20of%2049%20healthy%20women%20%2819-35%5Cu00a0years%29%20were%20included.%20In%20both%20gropus%20body%20mass%20index%20%28BMI%29%20was%20calculated%20and%20waist%20circumference%20%28WC%29%20was%20measured.%20Hair%20cortisol%2C%20total%20serum%20testosterone%20%28TT%29%2C%20serum%20cortisol%2C%2025%20OH%20vitamin%20D%20%2825OHD%29%2C%20insulin%2C%20high%20sensitivity%20C-reactive%20protein%20%28hsCRP%29%2C%20triglycerides%20%28TG%29%2C%20HDL%20cholesterol%20%28HDL%29%2C%20glucose%20and%20leptin%20were%20measured.%20Bioavailable%20testosterone%20%28bioT%29%20was%20calculated.%20Hair%20cortisol%20concentration%20was%20higher%20and%20significantly%20different%20in%20PCOS%20patients%20compared%20to%20the%20control%20group%20%28130%20vs%2063%5Cu00a0pg%5C%2Fmg%20of%20hair%2C%20p%5Cu2009%26lt%3B%5Cu20090.001%29.%20Subsequently%2C%20patients%20with%20PCOS%20were%20divided%20into%20two%20groups%20according%20to%20hair%20cortisol%20levels%3A%20group%201%20with%20normal%20hair%20cortisol%20concentration%20and%20group%202%20with%20levels%20above%20the%20upper%20limit%20of%20the%20reference%20values%20%28128%5Cu00a0pg%5C%2Fmg%20of%20hair%29.%20In%20group%202%2C%20TT%20significantly%20correlated%20with%2025OHD%2C%20hsCRP%2C%20TG%5C%2FHDL%20index%2C%20BMI%2C%20WC%2C%20insulin%20and%20HOMA%20%28p%5Cu2009%26lt%3B%5Cu20090.05%29%3B%20bioT%20correlated%20with%20hsCRP%20and%20leptin%20%28p%5Cu2009%26lt%3B%5Cu20090.05%29.%20Finally%2C%2025OHD%20was%20inversely%20correlated%20with%20leptin%20and%20with%20TG%5C%2FHDL%20index%20%28p%5Cu2009%26lt%3B%5Cu20090.05%29.%20High%20hair%20cortisol%20concentration%20in%20patients%20with%20PCOS%20confirmed%20hyperactivation%20of%20the%20HPA%20axis.%20The%20associations%20observed%20were%20only%20found%20in%20patients%20with%20PCOS%20with%20high%20hair%20cortisol%20levels%20%28%26gt%3B%5Cu2009128%5Cu00a0pg%5C%2Fmg%20of%20hair%29%2C%20showing%20a%20possible%20effect%20of%20HPA%20axis%20in%20these%20associations.%22%2C%22date%22%3A%222022-06-20%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1038%5C%2Fs41598-022-14061-9%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222045-2322%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A55%3A38Z%22%7D%7D%2C%7B%22key%22%3A%22JCL5MIRB%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Jiang%20et%20al.%22%2C%22parsedDate%22%3A%222022-12-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BJiang%20VS%2C%20Hawkins%20SD%2C%20McMichael%20A.%20Female%20pattern%20hair%20loss%20and%20polycystic%20ovarian%20syndrome%3A%20more%20than%20just%20hirsutism.%20Curr%20Opin%20Endocrinol%20Diabetes%20Obes.%202022%20Dec%201%3B29%286%29%3A535%26%23x2013%3B40.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Female%20pattern%20hair%20loss%20and%20polycystic%20ovarian%20syndrome%3A%20more%20than%20just%20hirsutism%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Victoria%20S.%22%2C%22lastName%22%3A%22Jiang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Spencer%20D.%22%2C%22lastName%22%3A%22Hawkins%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Amy%22%2C%22lastName%22%3A%22McMichael%22%7D%5D%2C%22abstractNote%22%3A%22PURPOSE%20OF%20REVIEW%3A%20To%20explore%20the%20recent%20updates%20in%20the%20diagnosis%2C%20management%2C%20and%20clinical%20implications%20of%20androgenic%20alopecia%20among%20patients%20diagnosed%20with%20polycystic%20ovarian%20syndrome%20%28PCOS%29.%5CnRECENT%20FINDINGS%3A%20PCOS%20diagnosis%20continues%20to%20be%20the%20most%20common%20cause%20of%20infertility%20among%20reproductively%20aged%20women%2C%20serving%20as%20the%20most%20common%20endocrinopathy%20among%20this%20population.%20Female%20pattern%20hair%20loss%20%28FPHL%29%20has%20been%20seen%20to%20be%20associated%20and%20more%20common%20among%20patients%20with%20PCOS%2C%20however%2C%20there%20are%20limited%20studies%20examining%20the%20impact%20of%20FPHL%20among%20PCOS%20patients.%20Although%20hyperandrogenism%20is%20associated%20with%20FPHL%2C%20the%20pathophysiology%20continues%20to%20be%20unclear%20as%20FPHL%20can%20be%20present%20with%20normal%20biochemical%20androgen%20markers.%20Treatment%20can%20be%20complex%2C%20as%20common%20treatments%20to%20promote%20hair%20growth%20can%20exacerbate%20undesired%20hirsutism%2C%20which%20can%20be%20overcome%20by%20cosmetic%20treatments.%20New%20second-line%20treatment%20options%20such%20as%20low%20level%20laser%20therapy%20and%20platelet%20rich%20plasma%20have%20been%20emerging%2C%20with%20limited%20data%20supporting%20efficacy.%5CnSUMMARY%3A%20PCOS%20is%20a%20complex%20endocrinological%20disorder%20that%20has%20significant%20gynecologic%2C%20cutaneous%2C%20and%20metabolic%20implications%20that%20require%20multidisciplinary%20collaboration%20and%20care.%20Reproductive%20goals%20should%20be%20thoroughly%20discussed%20prior%20to%20starting%20any%20treatment%2C%20as%20PCOS%20is%20the%20most%20common%20cause%20of%20infertility%20among%20reproductively-aged%20women.%22%2C%22date%22%3A%222022-12-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1097%5C%2FMED.0000000000000777%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221752-2978%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A54%3A08Z%22%7D%7D%2C%7B%22key%22%3A%22YYIJD3F9%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Klein%20et%20al.%22%2C%22parsedDate%22%3A%222023-01-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BKlein%20EJ%2C%20Oh%20CS%2C%20Karim%20M%2C%20Shapiro%20J%2C%20Lo%20Sicco%20K.%20A%20practical%20approach%20to%20the%20management%20of%20hair%20loss%20in%20patients%20with%20polycystic%20ovary%20syndrome.%20J%20Eur%20Acad%20Dermatol%20Venereol.%202023%20Jan%206%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20practical%20approach%20to%20the%20management%20of%20hair%20loss%20in%20patients%20with%20polycystic%20ovary%20syndrome%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elizabeth%20J.%22%2C%22lastName%22%3A%22Klein%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christina%20S.%22%2C%22lastName%22%3A%22Oh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%22%2C%22lastName%22%3A%22Karim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jerry%22%2C%22lastName%22%3A%22Shapiro%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kristen%22%2C%22lastName%22%3A%22Lo%20Sicco%22%7D%5D%2C%22abstractNote%22%3A%22Female%20patterned%20hair%20loss%20%28FPHL%29%20is%20a%20common%20form%20of%20androgenetic%20alopecia%20in%20women%20and%20is%20characterized%20by%20a%20hormonally%20directed%20diffuse%20hair%20loss%20on%20the%20scalp.%20Management%20of%20FPHL%20is%20well%20described%20in%20the%20literature%3B%20however%2C%20treatment%20of%20FPHL%20in%20patients%20with%20co-morbid%20polycystic%20ovarian%20syndrome%20%28PCOS%29%2C%20an%20endocrinologic%20condition%20found%20in%20reproductive-aged%20women%2C%20has%20not%20yet%20been%20reviewed.%20Due%20to%20the%20different%20pathomechanism%20of%20the%20diseases%20and%20complexity%20of%20FPHL%20in%20PCOS%20patients%2C%20this%20study%20aimed%20to%20review%20current%20diagnosis%20and%20management%20approaches%20for%20hair%20loss%20in%20PCOS%20patients%20specifically%20and%20highlight%20the%20growing%20need%20for%20more%20research%20in%20this%20growing%20patient%20population.%22%2C%22date%22%3A%222023-01-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fjdv.18842%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221468-3083%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A51%3A11Z%22%7D%7D%2C%7B%22key%22%3A%229IHCZSE6%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rayner%20et%20al.%22%2C%22parsedDate%22%3A%222025-12%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRayner%20DG%2C%20McMullen%20E%2C%20Mundle%20K%2C%20Pham%20M%2C%20Sibbald%20C%2C%20Donovan%20J.%20Bi-directional%20association%20between%20female%20pattern%20hair%20loss%20and%20polycystic%20ovary%20syndrome%3A%20A%20systematic%20review%20and%20meta-analysis.%20JAAD%20Int.%202025%20Dec%3B23%3A24%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Bi-directional%20association%20between%20female%20pattern%20hair%20loss%20and%20polycystic%20ovary%20syndrome%3A%20A%20systematic%20review%20and%20meta-analysis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Daniel%20G.%22%2C%22lastName%22%3A%22Rayner%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eric%22%2C%22lastName%22%3A%22McMullen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kshitija%22%2C%22lastName%22%3A%22Mundle%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Michelle%22%2C%22lastName%22%3A%22Pham%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cathryn%22%2C%22lastName%22%3A%22Sibbald%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeffrey%22%2C%22lastName%22%3A%22Donovan%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222025-12%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jdin.2025.08.004%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222666-3287%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226ZJHTIP4%22%5D%2C%22dateModified%22%3A%222026-01-02T14%3A45%3A22Z%22%7D%7D%5D%7D 1.
Miyazaki M, Takayasu S, Karakawa T, Aono T, Kurachi K, Matsumoto K. Activity of testosterone 5alpha-reductase in the hair follicles of women with polycystic ovaries. J Endocrinol. 1978 Sept;78(3):445–6.
1.
Futterweit W, Dunaif A, Yeh HC, Kingsley P. The prevalence of hyperandrogenism in 109 consecutive female patients with diffuse alopecia. J Am Acad Dermatol. 1988 Nov;19(5 Pt 1):831–6.
1.
Jakimiuk AJ, Weitsman SR, Magoffin DA. 5alpha-reductase activity in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1999 July;84(7):2414–8.
1.
Birch MP, Messenger JF, Messenger AG. Hair density, hair diameter and the prevalence of female pattern hair loss. Br J Dermatol. 2001 Feb;144(2):297–304.
1.
Cela E, Robertson C, Rush K, Kousta E, White DM, Wilson H, et al. Prevalence of polycystic ovaries in women with androgenic alopecia. Eur J Endocrinol. 2003 Nov;149(5):439–42.
1.
Azziz R, Sanchez LA, Knochenhauer ES, Moran C, Lazenby J, Stephens KC, et al. Androgen excess in women: experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004 Feb;89(2):453–62.
1.
Carmina E, Rosato F, Jannì A, Rizzo M, Longo RA. Extensive clinical experience: relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism. J Clin Endocrinol Metab. 2006 Jan;91(1):2–6.
1.
Quinn M, Shinkai K, Pasch L, Kuzmich L, Cedars M, Huddleston H. Prevalence of androgenic alopecia in patients with polycystic ovary syndrome and characterization of associated clinical and biochemical features. Fertil Steril. 2014 Apr;101(4):1129–34.
1.
Prasad S, De Souza B, Burns LJ, Lippincott M, Senna MM. Polycystic ovary syndrome in patients with hair thinning. J Am Acad Dermatol. 2020 July;83(1):260–1.
1.
Gonzalez D, Maidana P, Ibar C, Jamardo J, Jacobsen D, Fritzler A, et al. Hair cortisol in polycystic ovary syndrome. Sci Rep. 2022 June 20;12(1):10309.
1.
Jiang VS, Hawkins SD, McMichael A. Female pattern hair loss and polycystic ovarian syndrome: more than just hirsutism. Curr Opin Endocrinol Diabetes Obes. 2022 Dec 1;29(6):535–40.
1.
Klein EJ, Oh CS, Karim M, Shapiro J, Lo Sicco K. A practical approach to the management of hair loss in patients with polycystic ovary syndrome. J Eur Acad Dermatol Venereol. 2023 Jan 6;
1.
Rayner DG, McMullen E, Mundle K, Pham M, Sibbald C, Donovan J. Bi-directional association between female pattern hair loss and polycystic ovary syndrome: A systematic review and meta-analysis. JAAD Int. 2025 Dec;23:24–6.