Anagen effluvium is a form of non-scarring hair loss resulting from an insult to the rapidly dividing cells within the hair follicle during the anagen (growth) phase of the hair cycle. While the most widely recognized cause is cytotoxic chemotherapy, a variety of other drugs can precipitate this condition. This article explores the underlying biology of anagen effluvium, delineates the spectrum of pharmacologic agents capable of inducing it, outlines clinical presentation and diagnostic considerations, and discusses current strategies for management and mitigation.
The Hair Growth Cycle and Anagen Effluvium: Human scalp hair follicles undergo a cyclical process comprising three principal stages: anagen (active growth), catagen (regression), and telogen (resting). The anagen phase lasts two to six years and is characterized by intense cellular proliferation in the hair matrix, generating the hair shaft. Any disruption of mitotic activity within these matrix keratinocytes can precipitate abrupt hair follicle dysfunction, leading to anagen effluvium.
In anagen effluvium, insult to the follicular matrix arrests cell division, impairing hair shaft formation. Within days to weeks, weakened hair shafts break off or are forcibly expelled, resulting in diffuse, often rapid, shedding of scalp hair – and potentially eyebrows, eyelashes, and body hair as well. Unlike telogen effluvium (where affected hairs enter the resting phase and shed months later), anagen effluvium develops within days of exposure to the causative insult.
Pathophysiology of Drug-Induced Anagen Effluvium: The rapid turnover of matrix keratinocytes renders them particularly vulnerable to agents that impair DNA synthesis, mitosis, or protein assembly. Key mechanisms include:
DNA Damage and Repair Inhibition Alkylating agents (e.g., cyclophosphamide, busulfan) form DNA cross-links, triggering apoptosis of proliferating cells.Antimetabolites (e.g., methotrexate, 5-fluorouracil) inhibit nucleotide synthesis, leading to stalled replication forks and cell death. Microtubule Disruption Vinca alkaloids (e.g., vincristine, vinblastine) and taxanes (e.g., paclitaxel, docetaxel) interfere with tubulin polymerization or depolymerization, respectively, interrupting the mitotic spindle apparatus inside cells. Protein Synthesis and Signaling Interference Proteasome inhibitors (e.g., bortezomib) alter protein turnover, while certain tyrosine kinase inhibitors (e.g., imatinib) may disrupt signaling pathways essential for follicular cell survival. Mitochondrial and Oxidative Stress Some agents induce mitochondrial dysfunction or generate reactive oxygen species, exacerbating apoptosis within the hair follicle bulb. The degree of hair loss depends on the type of agent, dosage, route and duration of administration, and individual patient susceptibility. Cumulative dosing and combination regimens – common in oncology – often compound the effect.
Pharmacologic Agents Commonly Implicated: While cytotoxic chemotherapy remains the archetypal trigger, a broader array of medications can induce anagen effluvium:
Chemotherapeutic Drugs Alkylating agents: Cyclophosphamide, melphalan, busulfan.Antimetabolites: Methotrexate, 5-FU, cytarabine.Anti-microtubule agents: Vincristine, vinorelbine, paclitaxel, docetaxel.Anthracyclines: Doxorubicin, epirubicin. Targeted Therapies and Biologics EGFR inhibitors: Erlotinib, cetuximab (although more commonly cause brittle hair and changes in hair curl).Proteasome inhibitors: Bortezomib.Immune checkpoint inhibitors: Rare, but case reports exist. Non-Oncologic Drugs Antithyroid agents: Methimazole, propylthiouracil – through poorly understood mechanisms.Retinoids: High-dose isotretinoin can occasionally induce anagen arrest.Anticoagulants: Heparin and warfarin – typically associated with telogen effluvium, but rare reports of anagen effluvium involvement exist. It is essential for clinicians to review a patient’s complete medication history, as combination therapies may have synergistic effects on follicular toxicity.
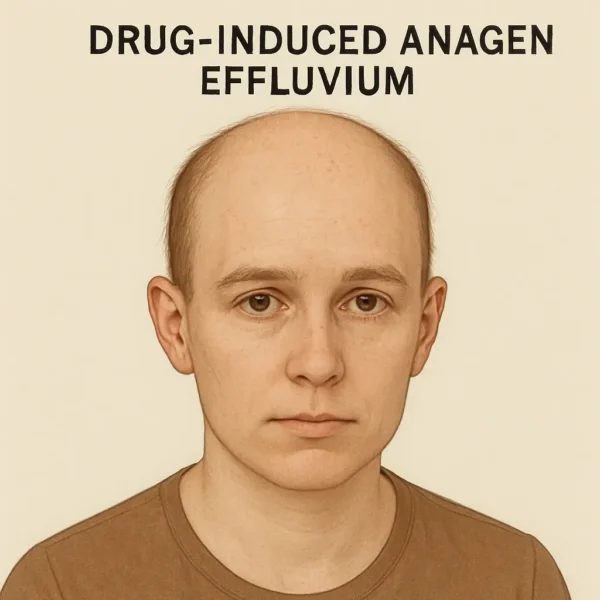
Clinical Presentation – Timing and Pattern: Anagen effluvium typically presents as diffuse hair shedding within 7–14 days of initiating the offending agent. Hair loss may commence as early as 3–5 days in highly cytotoxic regimens. The shedding often affects at least 50% of scalp hair, and involvement of eyebrows, eyelashes, axillary, and pubic hair is common.
Diagnosis – Scalp Examination:
Hair Pull Test: Gentle traction on small tufts yields an elevated number of hairs (< 10% is typical), predominantly broken hairs with tapered ends.Trichoscopy: May reveal exclamation-mark hairs – short hairs narrower at the base – though these are more characteristic of alopecia areata, they can also be observed in anagen effluvium. Histopathology:
Skin Biopsy: Usually a skin biopsy is not required as anagen effluvium is clinically fairly obvious. However if performed, a biopsy shows dystrophic anagen follicles, absence of any significant inflammatory infiltrate, and intact dermal structures (indicating non-scarring hair loss). Biopsy is not required unless diagnostic uncertainty exists. Differential Diagnosis:
Telogen Effluvium: Typically presents 2–4 months after the initiating event.Alopecia Areata: Patchy loss, exclamation-mark hairs, potential nail involvement.Androgenetic Alopecia: Gradual thinning in characteristic distribution, miniaturized follicles. Management Strategies: Given the distressing nature of rapid hair loss, a multifaceted approach is required:
Scalp Cooling (Cryotherapy): Application of cooled caps during chemotherapy reduces scalp blood flow and follicular uptake of cytotoxic drugs. Numerous trials report a 50–70% reduction in hair loss severity, with highest efficacy in taxane- and anthracycline-based regimens. Limitations include patient discomfort, logistical demands, and risk of scalp metastases (this is a theoretical concern, it has not been substantiated by large studies).Pharmacologic Agents: Topical application of Minoxidil (2–5%) may accelerate regrowth post-therapy but it does not prevent initial shedding. Anti-apoptotic Agents: Experimental compounds (e.g., ASK1 inhibitors) are under investigation to protect follicular keratinocytes. Symptomatic and Supportive Care:
Camouflage Techniques: Wigs, turbans, scarves, and cosmetic styling (e.g., eyebrow pencils). Early referral to a wig-fitting service is recommended prior to hair loss onset.Psychological Support: Hair loss can significantly impair quality of life and self-image; counseling and support groups may alleviate distress. Treatment of Underlying Cause:
Dose Modification: When feasible, dose reduction or alteration of the offending agent may attenuate hair loss. This decision must balance with oncologic efficacy or disease control – against patient preference and quality of life considerations.Drug Substitution: Switching to less folliculotoxic therapies may be possible in non-oncologic contexts (e.g., alternative antithyroid regimens). Promoting Regrowth: After cessation of the causative drug, anagen effluvium typically reverses, and hair regrowth begins within 1–3 months. Full regrowth, including restoration of color and texture, may take 6–12 months. In most cases, regrown hair initially appears finer and lighter (vellus-like), gradually normalizing over successive hair cycles.
Prognosis and Long-Term Outcomes: Drug-induced anagen effluvium is generally reversible, with no permanent follicular damage or scarring. Occasionally however, prolonged or high-dose exposures can result in incomplete recovery or persistent thinning. Monitoring and long-term follow-up can ensure timely identification of any atypical or protracted courses.
Future Directions and Research: Emerging strategies aim to elucidate molecular targets for follicular protection:
Cytokine and Growth Factor Modulation: Investigating granulocyte-macrophage colony-stimulating factor (GM-CSF) and fibroblast growth factor (FGF) analogues to promote follicle resilience.Gene Therapy: Targeted delivery of anti-apoptotic genes to the hair bulb holds theoretical promise.Topical Nanoparticles: Enhancing delivery of protective agents directly to follicular cells without systemic exposure. Clinical trials remain sparse, particularly outside oncology contexts. Collaboration between dermatologists, oncologists, and pharmacologists is critical to develop standardized prevention protocols and to validate candidate protective agents.
Conclusion: Drug-induced anagen effluvium represents a distressing but largely reversible form of hair loss, predominantly encountered in patients receiving cytotoxic chemotherapy but also associated with diverse pharmacologic agents. A clear understanding of the hair cycle, the mechanisms of follicular injury, and the spectrum of causative drugs enables clinicians to counsel patients effectively, implement preventive measures such as scalp cooling, and provide supportive care throughout the course of treatment. While current management focuses on mitigation and symptomatic relief, ongoing research into follicle-protective therapies offers hope for more robust prophylactic interventions in the future. The multidisciplinary collaboration and patient-centered approach remain central to optimizing outcomes for individuals affected by this challenging condition.
Bibliography
11711645 {11711645:RI4AV3P9},{11711645:PEM2GXVP},{11711645:FI5ZMWAG},{11711645:675CJQ37},{11711645:GHBY9GHK},{11711645:HX3TSHPM},{11711645:E5LRJP5D},{11711645:VB5P8INQ},{11711645:SD2ZRWVF},{11711645:XM6PEZ2V},{11711645:MLE43I3Q},{11711645:D63N7YQG},{11711645:BP68Y65B},{11711645:4C8AKA3P},{11711645:V9P3BUD5} 1 vancouver 50 date asc 1839 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22RI4AV3P9%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Duvic%20et%20al.%22%2C%22parsedDate%22%3A%221996-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDuvic%20M%2C%20Lemak%20NA%2C%20Valero%20V%2C%20Hymes%20SR%2C%20Farmer%20KL%2C%20Hortobagyi%20GN%2C%20et%20al.%20A%20randomized%20trial%20of%20minoxidil%20in%20chemotherapy-induced%20alopecia.%20J%20Am%20Acad%20Dermatol.%201996%20July%3B35%281%29%3A74%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20randomized%20trial%20of%20minoxidil%20in%20chemotherapy-induced%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Duvic%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22N.%20A.%22%2C%22lastName%22%3A%22Lemak%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22V.%22%2C%22lastName%22%3A%22Valero%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%20R.%22%2C%22lastName%22%3A%22Hymes%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%20L.%22%2C%22lastName%22%3A%22Farmer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G.%20N.%22%2C%22lastName%22%3A%22Hortobagyi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%20J.%22%2C%22lastName%22%3A%22Trancik%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20A.%22%2C%22lastName%22%3A%22Bandstra%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%20D.%22%2C%22lastName%22%3A%22Compton%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Hair%20loss%20is%20a%20side%20effect%20of%20many%20chemotherapeutic%20agents%2C%20and%20patients%20have%20even%20refused%20possibly%20palliative%20or%20lifesaving%20drugs%20because%20they%20could%20not%20accept%20temporary%20or%20prolonged%20baldness.%20Topical%20minoxidil%20has%20been%20shown%20to%20be%20effective%20for%20androgenetic%20alopecia%20and%20alopecia%20areata.%5CnOBJECTIVE%3A%20Our%20purpose%20was%20to%20investigate%20the%20value%20and%20safety%20of%20minoxidil%20in%20chemotherapy-induced%20hair%20loss.%5CnMETHODS%3A%20Twenty-two%20women%20who%20were%20facing%20adjuvant%20chemotherapy%20after%20breast%20surgery%20were%20registered%20in%20a%20protocol%20that%20used%20a%202%25%20minoxidil%20topical%20solution%20or%20a%20placebo%20in%20a%20randomized%20double-blind%20trial.%5CnRESULTS%3A%20There%20was%20a%20statistically%20significant%20difference%20%28favoring%20minoxidil%29%20in%20the%20interval%20from%20maximal%20hair%20loss%20to%20first%20regrowth.%20Thus%20the%20period%20of%20baldness%20was%20shortened%20%28mean%2C%2050.2%20days%29%20in%20the%20minoxidil%20group.%5CnCONCLUSION%3A%20Minoxidil%20decreased%20the%20duration%20of%20alopecia%20caused%20by%20chemotherapy.%20There%20were%20no%20significant%20side%20effects.%22%2C%22date%22%3A%221996-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2FS0190-9622%2896%2990500-9%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220190-9622%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A42%3A10Z%22%7D%7D%2C%7B%22key%22%3A%22PEM2GXVP%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Sharma%20et%20al.%22%2C%22parsedDate%22%3A%222001-12%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSharma%20PK%2C%20Gautam%20RK%2C%20Bhardwaj%20M%2C%20Kar%20HK.%20Isonicotinic%20acid%20hydrazide%20induced%20anagen%20effluvium%20and%20associated%20lichenoid%20eruption.%20J%20Dermatol.%202001%20Dec%3B28%2812%29%3A737%26%23x2013%3B41.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Isonicotinic%20acid%20hydrazide%20induced%20anagen%20effluvium%20and%20associated%20lichenoid%20eruption%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%20K.%22%2C%22lastName%22%3A%22Sharma%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%20K.%22%2C%22lastName%22%3A%22Gautam%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Bhardwaj%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22H.%20K.%22%2C%22lastName%22%3A%22Kar%22%7D%5D%2C%22abstractNote%22%3A%22A%2032%20year-old%20woman%20developed%20generalised%20lichenoid%20eruptions%20on%20her%20body%20followed%20by%20diffuse%20loss%20of%20scalp%20hair%20of%20the%20anagen%20effluvium%20type.%20She%20was%20receiving%20several%20anti-tubercular%20drugs%2C%20including%20rifampicin%2C%20isonicotinic%20acid%20hydrazide%20%28INH%29%2C%20pyrazinamide%2C%20and%20ethambutol%2C%20for%20abdominal%20tuberculosis.%20INH%2C%20which%20is%20a%20leading%20cause%20of%20drug%20eruptions%20in%20the%20above%20group%20of%20drugs%20was%20withdrawn.%20However%2C%20the%20other%20antitubercular%20drugs%20were%20continued%20along%20with%2040%20mg%20of%20prednisolone%20in%20a%20single%20daily%20morning%20dose.%20The%20latter%20was%20discontinued%20slowly%20over%20a%20period%20of%2010%20weeks.%20There%20was%20complete%20recovery%20of%20hair%20loss%20and%20the%20regrowth%20started%20after%2012%20weeks%20of%20alopecia.%20Such%20anagen%20effluvium%20with%20lichenoid%20eruption%20following%20INH%20therapy%20has%20not%20been%20observed%20previously.%20The%20complete%20recovery%20from%20anagen%20effluvium%20is%20difficult%20to%20explain%2C%20but%20it%20could%20have%20been%20because%20of%20the%20early%20initiation%20of%20corticosteroid.%22%2C%22date%22%3A%222001-12%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220385-2407%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A45%3A07Z%22%7D%7D%2C%7B%22key%22%3A%22FI5ZMWAG%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Yun%20and%20Kim%22%2C%22parsedDate%22%3A%222007%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BYun%20SJ%2C%20Kim%20SJ.%20Hair%20loss%20pattern%20due%20to%20chemotherapy-induced%20anagen%20effluvium%3A%20a%20cross-sectional%20observation.%20Dermatology.%202007%3B215%281%29%3A36%26%23x2013%3B40.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hair%20loss%20pattern%20due%20to%20chemotherapy-induced%20anagen%20effluvium%3A%20a%20cross-sectional%20observation%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sook%20Jung%22%2C%22lastName%22%3A%22Yun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Seong-Jin%22%2C%22lastName%22%3A%22Kim%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Anagen%20effluvium%20is%20a%20common%20side%20effect%20of%20chemotherapy%2C%20but%20few%20studies%20have%20examined%20its%20clinical%20characteristics.%5CnOBJECTIVE%3A%20This%20study%20was%20aimed%20at%20evaluating%20the%20hair%20loss%20caused%20by%20chemotherapeutic%20agents.%5CnMETHODS%3A%20Sixty-four%20patients%20with%20anagen%20effluvium%20were%20evaluated%20in%20the%20study.%20Chemotherapeutic%20agents%20were%20classified%20into%205%20different%20groups.%20The%20pattern%20of%20hair%20loss%20was%20analyzed%20when%20specific%20involvement%20of%20the%20hairline%20was%20obvious.%5CnRESULTS%3A%20Forty-six%20%2871.9%25%29%20of%20the%2064%20total%20patients%20maintained%20hairs%20along%20their%20hairline.%20Hairs%20were%20maintained%20with%20a%20total%20hairline%20in%2020%20%2831.3%25%29%2C%20frontal%20hairline%20in%2013%20%2820.3%25%29%20and%20occipital%20hairline%20in%2012%20%2818.8%25%29%20patients.%20Among%20the%2020%20males%20with%20patterned%20hair%20loss%2C%20the%20following%20hairlines%20were%20preserved%3A%20occipital%20in%2010%20%2850%25%29%2C%20total%20in%207%20%2835%25%29%20and%20frontal%20in%203%20%2815%25%29.%20Among%20the%2025%20females%20with%20patterned%20hair%20loss%2C%20hairlines%20were%20preserved%20as%20total%20in%2013%20%2852%25%29%2C%20frontal%20in%2010%20%2840%25%29%20and%20occipital%20in%202%20%288%25%29.%20However%2C%20no%20significant%20differences%20were%20detected%20in%20hair%20loss%20patterns%20according%20to%20age%2C%20associated%20symptoms%2C%20chemotherapeutic%20agent%20group%20or%20combination%20of%20chemotherapeutic%20agents.%5CnCONCLUSION%3A%20Our%20results%20suggest%20that%20anagen%20effluvium%20induced%20by%20chemotherapeutic%20agents%20represents%20patterned%20hair%20loss.%22%2C%22date%22%3A%222007%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1159%5C%2F000102031%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221421-9832%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A38%3A58Z%22%7D%7D%2C%7B%22key%22%3A%22675CJQ37%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Tallon%20et%20al.%22%2C%22parsedDate%22%3A%222010-08%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BTallon%20B%2C%20Blanchard%20E%2C%20Goldberg%20LJ.%20Permanent%20chemotherapy-induced%20alopecia%3A%20case%20report%20and%20review%20of%20the%20literature.%20J%20Am%20Acad%20Dermatol.%202010%20Aug%3B63%282%29%3A333%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Permanent%20chemotherapy-induced%20alopecia%3A%20case%20report%20and%20review%20of%20the%20literature%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ben%22%2C%22lastName%22%3A%22Tallon%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elizabeth%22%2C%22lastName%22%3A%22Blanchard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lynne%20J.%22%2C%22lastName%22%3A%22Goldberg%22%7D%5D%2C%22abstractNote%22%3A%22Reversible%20alopecia%20following%20chemotherapy%20is%20well%20recognized%20and%20typically%20not%20evaluated%20by%20dermatologists.%20However%2C%20there%20are%20an%20increasing%20number%20of%20reports%20of%20permanent%20chemotherapy-induced%20alopecia%2C%20typically%20following%20high-dose%20chemotherapy%20and%20subsequent%20bone%20marrow%20transplantation.%20We%20describe%20an%20unusual%20case%20of%20permanent%20alopecia%20in%20a%20patient%20who%20received%20adjuvant%20chemotherapy%20for%20breast%20carcinoma%2C%20and%20not%20a%20conditioning%20regimen%20before%20bone%20marrow%20transplantation.%20A%20unique%20histologic%20finding%20of%20replacement%20of%20anagen%20hair%20follicles%20by%20linear%20columns%20of%20basaloid%20epithelium%20is%20reported.%20We%20review%20the%20clinical%20and%20histologic%20findings%20of%20permanent%20chemotherapy-induced%20alopecia%20and%20speculate%20on%20its%20pathogenesis.%22%2C%22date%22%3A%222010-08%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2009.06.063%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A40%3A13Z%22%7D%7D%2C%7B%22key%22%3A%22GHBY9GHK%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Yeager%20and%20Olsen%22%2C%22parsedDate%22%3A%222011%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BYeager%20CE%2C%20Olsen%20EA.%20Treatment%20of%20chemotherapy-induced%20alopecia.%20Dermatol%20Ther.%202011%3B24%284%29%3A432%26%23x2013%3B42.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Treatment%20of%20chemotherapy-induced%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Caroline%20E.%22%2C%22lastName%22%3A%22Yeager%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Elise%20A.%22%2C%22lastName%22%3A%22Olsen%22%7D%5D%2C%22abstractNote%22%3A%22Chemotherapy-induced%20alopecia%20has%20been%20well%20documented%20as%20a%20cause%20of%20distress%20to%20patients%20undergoing%20cancer%20treatment.%20Despite%20the%20importance%20of%20hair%20loss%20to%20patients%2C%20however%2C%20patients%20often%20receive%20little%20more%20counseling%20than%20the%20advice%20to%20purchase%20a%20wig%20or%20other%20head%20covering%20for%20the%20duration%20of%20their%20treatment.%20Research%20into%20non-camouflage%20%28wigs%2C%20turbans%2C%20and%20head%20scarves%29%20treatment%20methods%20has%20been%20complicated%20both%20by%20a%20lack%20of%20a%20standardized%20methodology%20for%20evaluating%20hair%20loss%20and%20hair%20regrowth%20and%20by%20a%20lack%20of%20human%20trials.%20Nevertheless%2C%20scalp%20cooling%20as%20a%20method%20of%20preventing%20hair%20loss%20during%20chemotherapy%20and%202%25%20topical%20minoxidil%20as%20a%20therapy%20for%20accelerating%20regrowth%20after%20chemotherapy%20are%20both%20effective%20non-camouflage%20options%20for%20treatment.%20Other%20proposed%20treatments%20for%20prevention%20of%20hair%20loss%20during%20chemotherapy%20have%20demonstrated%20promise%20in%20early%20trials%2C%20but%20these%20findings%20will%20need%20validation%20from%20rigorous%20further%20studies.%20The%20increasing%20number%20of%20reports%20of%20permanent%20alopecia%20not%20just%20with%20pre-bone%20marrow%20transplant%2C%20high-dose%20busulfan%2C%20and%20cyclophosphamide%20regimens%20but%20also%20with%20standard%20breast%20cancer%20chemotherapy%20regimens%20illustrates%20the%20importance%20of%20further%20research%20into%20treatment%20methods%20for%20chemotherapy-induced%20alopecia.%22%2C%22date%22%3A%222011%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1529-8019.2011.01430.x%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221529-8019%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A41%3A03Z%22%7D%7D%2C%7B%22key%22%3A%22HX3TSHPM%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Curto-Barredo%20et%20al.%22%2C%22parsedDate%22%3A%222015-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCurto-Barredo%20L%2C%20Segura%20S%2C%20Mart%26%23xED%3Bn-Ezquerra%20G%2C%20Lloveras%20B%2C%20Gallardo%20F%2C%20Pujol%20RM.%20Anagen%20effluvium%20due%20to%20thallium%20poisoning%20derived%20from%20the%20intake%20of%20Chinese%20herbal%20medicine%20and%20rodenticide%20containing%20thallium%20salts.%20J%20Dermatol.%202015%20Oct%3B42%2810%29%3A1027%26%23x2013%3B9.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anagen%20effluvium%20due%20to%20thallium%20poisoning%20derived%20from%20the%20intake%20of%20Chinese%20herbal%20medicine%20and%20rodenticide%20containing%20thallium%20salts%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Laia%22%2C%22lastName%22%3A%22Curto-Barredo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S%5Cu00f2nia%22%2C%22lastName%22%3A%22Segura%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gemma%22%2C%22lastName%22%3A%22Mart%5Cu00edn-Ezquerra%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Belen%22%2C%22lastName%22%3A%22Lloveras%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fernando%22%2C%22lastName%22%3A%22Gallardo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ramon%20M.%22%2C%22lastName%22%3A%22Pujol%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015-10%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2F1346-8138.12997%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221346-8138%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A44%3A45Z%22%7D%7D%2C%7B%22key%22%3A%22VB5P8INQ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Bains%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BBains%20A%2C%20Verma%20GK%2C%20Vedant%20D%2C%20Negi%20A.%20Anagen%20effluvium%20secondary%20to%20Gloriosa%20superba%20ingestion.%20Indian%20J%20Dermatol%20Venereol%20Leprol.%202016%3B82%286%29%3A677%26%23x2013%3B80.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anagen%20effluvium%20secondary%20to%20Gloriosa%20superba%20ingestion%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Anupama%22%2C%22lastName%22%3A%22Bains%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G.%20K.%22%2C%22lastName%22%3A%22Verma%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Deepak%22%2C%22lastName%22%3A%22Vedant%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ajeet%22%2C%22lastName%22%3A%22Negi%22%7D%5D%2C%22abstractNote%22%3A%22Anagen%20effluvium%2C%20the%20shedding%20of%20anagen%20hair%2C%20leads%20to%20diffuse%20non-scarring%20alopecia.%20We%20report%20two%20cases%20of%20anagen%20effluvium%20in%20the%20same%20family%20secondary%20to%20the%20ingestion%20of%20tubers%20of%20Gloriosa%20superba%2C%20which%20contains%20the%20antimitotic%20alkaloid%20colchicine.%20Both%20patients%20developed%20anagen%20effluvium%20and%20gastroenteritis%201-2%20weeks%20after%20consuming%20the%20tubers.%20In%20addition%2C%20one%20of%20them%20had%20bicytopenia%2C%20pleural%20effusion%2C%20hematuria%20and%20altered%20liver%20function%20tests.%20Both%20were%20managed%20conservatively%20and%20counseled%20regarding%20the%20reversible%20nature%20of%20the%20hair%20loss.%20Follow-up%20at%203%20months%20showed%20regrowth%20of%20hair%20in%20both%20the%20cases.%22%2C%22date%22%3A%222016%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.4103%5C%2F0378-6323.186486%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220973-3922%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A38%3A07Z%22%7D%7D%2C%7B%22key%22%3A%22E5LRJP5D%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Combalia%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCombalia%20A%2C%20Baliu-Piqu%26%23xE9%3B%20C%2C%20Fortea%20A%2C%20Ferrando%20J.%20Anagen%20Effluvium%20Following%20Acute%20Colchicine%20Poisoning.%20Int%20J%20Trichology.%202016%3B8%284%29%3A171%26%23x2013%3B2.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anagen%20Effluvium%20Following%20Acute%20Colchicine%20Poisoning%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrea%22%2C%22lastName%22%3A%22Combalia%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Carola%22%2C%22lastName%22%3A%22Baliu-Piqu%5Cu00e9%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Adriana%22%2C%22lastName%22%3A%22Fortea%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Juan%22%2C%22lastName%22%3A%22Ferrando%22%7D%5D%2C%22abstractNote%22%3A%22We%20present%20a%20case%20of%20a%2017-year-old%20girl%20admitted%20to%20the%20Psychiatric%20Department%20recovering%20from%20a%20suicide%20attempt%20with%20colchicine.%20One%20week%20after%20poisoning%2C%20a%20sudden%20onset%20of%20hair%20loss%20was%20observed.%20Positive%20hair%20pull%20test%20and%20trichoscopy%20demonstrated%20the%20presence%20of%20anagen%20hairs%20with%20pigmented%20long%20roots%20covered%20by%20the%20root%20sheaths.%20Colchicine%20poisoning%20is%20an%20uncommon%2C%20but%20potentially%20life-threatening%20toxicologic%20emergency.%20An%20overdose%20of%20colchicine%20inhibits%20cell%20division%2C%20and%20thus%20the%20most%20affected%20organs%20are%20those%20which%20have%20a%20high%20rate%20of%20cell%20turnover.%20Hair%20loss%20resulting%20from%20colchicine%20poisoning%20presents%20as%20anagen%20effluvium%2C%20as%20it%20occurs%20with%20an%20exposure%20to%20toxic%20chemicals.%20Pharmacotherapy%20or%20specific%20treatment%20is%20not%20usually%20required%2C%20since%20the%20follicle%20resumes%20its%20normal%20activity%20after%20withdrawal%20of%20the%20antimitotic%20factors.%22%2C%22date%22%3A%222016%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.4103%5C%2F0974-7753.203171%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220974-7753%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A44%3A11Z%22%7D%7D%2C%7B%22key%22%3A%22SD2ZRWVF%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Campbell%20et%20al.%22%2C%22parsedDate%22%3A%222016-06-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCampbell%20C%2C%20Bahrami%20S%2C%20Owen%20C.%20Anagen%20Effluvium%20Caused%20by%20Thallium%20Poisoning.%20JAMA%20Dermatol.%202016%20June%201%3B152%286%29%3A724%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anagen%20Effluvium%20Caused%20by%20Thallium%20Poisoning%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Caren%22%2C%22lastName%22%3A%22Campbell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Soon%22%2C%22lastName%22%3A%22Bahrami%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cindy%22%2C%22lastName%22%3A%22Owen%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222016-06-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1001%5C%2Fjamadermatol.2016.0194%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222168-6084%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A38%3A20Z%22%7D%7D%2C%7B%22key%22%3A%22XM6PEZ2V%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Dunnill%20et%20al.%22%2C%22parsedDate%22%3A%222018-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDunnill%20CJ%2C%20Al-Tameemi%20W%2C%20Collett%20A%2C%20Haslam%20IS%2C%20Georgopoulos%20NT.%20A%20Clinical%20and%20Biological%20Guide%20for%20Understanding%20Chemotherapy-Induced%20Alopecia%20and%20Its%20Prevention.%20Oncologist.%202018%20Jan%3B23%281%29%3A84%26%23x2013%3B96.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20Clinical%20and%20Biological%20Guide%20for%20Understanding%20Chemotherapy-Induced%20Alopecia%20and%20Its%20Prevention%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christopher%20John%22%2C%22lastName%22%3A%22Dunnill%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wafaa%22%2C%22lastName%22%3A%22Al-Tameemi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrew%22%2C%22lastName%22%3A%22Collett%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Iain%20Stuart%22%2C%22lastName%22%3A%22Haslam%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nikolaos%20Theodoros%22%2C%22lastName%22%3A%22Georgopoulos%22%7D%5D%2C%22abstractNote%22%3A%22Chemotherapy-induced%20alopecia%20%28CIA%29%20is%20the%20most%20visibly%20distressing%20side%20effect%20of%20commonly%20administered%20chemotherapeutic%20agents.%20Because%20psychological%20health%20has%20huge%20relevance%20to%20lifestyle%2C%20diet%2C%20and%20self-esteem%2C%20it%20is%20important%20for%20clinicians%20to%20fully%20appreciate%20the%20psychological%20burden%20that%20CIA%20can%20place%20on%20patients.%20Here%2C%20for%20the%20first%20time%20to%20our%20knowledge%2C%20we%20provide%20a%20comprehensive%20review%20encompassing%20the%20molecular%20characteristics%20of%20the%20human%20hair%20follicle%20%28HF%29%2C%20how%20different%20anticancer%20agents%20damage%20the%20HF%20to%20cause%20CIA%2C%20and%20subsequent%20HF%20pathophysiology%2C%20and%20we%20assess%20known%20and%20emerging%20prevention%20modalities%20that%20have%20aimed%20to%20reduce%20or%20prevent%20CIA.%20We%20argue%20that%2C%20at%20present%2C%20scalp%20cooling%20is%20the%20only%20safe%20and%20U.S.%20Food%20and%20Drug%20Administration-cleared%20modality%20available%2C%20and%20we%20highlight%20the%20extensive%20available%20clinical%20and%20experimental%20%28biological%29%20evidence%20for%20its%20efficacy.%20The%20likelihood%20of%20a%20patient%20that%20uses%20scalp%20cooling%20during%20chemotherapy%20maintaining%20enough%20hair%20to%20not%20require%20a%20wig%20is%20approximately%2050%25.%20This%20is%20despite%20different%20types%20of%20chemotherapy%20regimens%2C%20patient-specific%20differences%2C%20and%20possible%20lack%20of%20staff%20experience%20in%20effectively%20delivering%20scalp%20cooling.%20The%20increased%20use%20of%20scalp%20cooling%20and%20an%20understanding%20of%20how%20to%20deliver%20it%20most%20effectively%20to%20patients%20has%20enormous%20potential%20to%20ease%20the%20psychological%20burden%20of%20CIA%2C%20until%20other%2C%20more%20efficacious%2C%20equally%20safe%20treatments%20become%20available.%5CnIMPLICATIONS%20FOR%20PRACTICE%3A%20Chemotherapy-induced%20alopecia%20%28CIA%29%20represents%20perhaps%20the%20most%20distressing%20side%20effect%20of%20chemotherapeutic%20agents%20and%20is%20of%20huge%20concern%20to%20the%20majority%20of%20patients.%20Scalp%20cooling%20is%20currently%20the%20only%20safe%20option%20to%20combat%20CIA.%20Clinical%20and%20biological%20evidence%20suggests%20improvements%20can%20be%20made%2C%20including%20efficacy%20in%20delivering%20adequately%20low%20temperature%20to%20the%20scalp%20and%20patient-specific%20cap%20design.%20The%20increased%20use%20of%20scalp%20cooling%2C%20an%20understanding%20of%20how%20to%20deliver%20it%20most%20effectively%2C%20and%20biological%20evidence-based%20approaches%20to%20improve%20its%20efficacy%20have%20enormous%20potential%20to%20ease%20the%20psychological%20burden%20of%20CIA%2C%20as%20this%20could%20lead%20to%20improvements%20in%20treatment%20and%20patient%20quality-of-life.%22%2C%22date%22%3A%222018-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1634%5C%2Ftheoncologist.2017-0263%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221549-490X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A43%3A04Z%22%7D%7D%2C%7B%22key%22%3A%22MLE43I3Q%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ghias%20et%20al.%22%2C%22parsedDate%22%3A%222020-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BGhias%20MH%2C%20Amin%20BD%2C%20Kutner%20AJ.%20Albendazole-induced%20anagen%20effluvium.%20JAAD%20Case%20Rep.%202020%20Jan%3B6%281%29%3A54%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Albendazole-induced%20anagen%20effluvium%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mondana%20H.%22%2C%22lastName%22%3A%22Ghias%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bijal%20D.%22%2C%22lastName%22%3A%22Amin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Allison%20J.%22%2C%22lastName%22%3A%22Kutner%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222020-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jdcr.2019.08.010%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222352-5126%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A37%3A56Z%22%7D%7D%2C%7B%22key%22%3A%22D63N7YQG%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Sharma%20et%20al.%22%2C%22parsedDate%22%3A%222022%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSharma%20R%2C%20Poddar%20S%2C%20Podder%20I.%20Azathioprine%20Induced%20Anagen%20Effluvium-%20An%20Uncommon%20Adverse%20Effect%20of%20a%20Commonly%20Used%20Drug.%20Indian%20J%20Dermatol.%202022%3B67%286%29%3A815%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Azathioprine%20Induced%20Anagen%20Effluvium-%20An%20Uncommon%20Adverse%20Effect%20of%20a%20Commonly%20Used%20Drug%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rashmi%22%2C%22lastName%22%3A%22Sharma%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Shreya%22%2C%22lastName%22%3A%22Poddar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Indrashis%22%2C%22lastName%22%3A%22Podder%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222022%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.4103%5C%2Fijd.ijd_497_22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221998-3611%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A45%3A25Z%22%7D%7D%2C%7B%22key%22%3A%22BP68Y65B%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Starace%20et%20al.%22%2C%22parsedDate%22%3A%222022-03%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BStarace%20M%2C%20Orlando%20G%2C%20Bruni%20F%2C%20Alessandrini%20A%2C%20Piraccini%20BM.%20Anagen%20effluvium%20and%20the%20role%20of%20trichoscopy.%20Clin%20Exp%20Dermatol.%202022%20Mar%3B47%283%29%3A589%26%23x2013%3B91.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anagen%20effluvium%20and%20the%20role%20of%20trichoscopy%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Starace%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G.%22%2C%22lastName%22%3A%22Orlando%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22F.%22%2C%22lastName%22%3A%22Bruni%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Alessandrini%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20M.%22%2C%22lastName%22%3A%22Piraccini%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222022-03%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fced.14982%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221365-2230%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A43%3A56Z%22%7D%7D%2C%7B%22key%22%3A%224C8AKA3P%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Saleh%20et%20al.%22%2C%22parsedDate%22%3A%222025%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSaleh%20D%2C%20Nassereddin%20A%2C%20Saleh%20HM%2C%20Cook%20C.%20Anagen%20Effluvium.%20In%3A%20StatPearls.%20Treasure%20Island%20%28FL%29%3A%20StatPearls%20Publishing%3B%202025.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22bookSection%22%2C%22title%22%3A%22Anagen%20Effluvium%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dahlia%22%2C%22lastName%22%3A%22Saleh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ali%22%2C%22lastName%22%3A%22Nassereddin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Haitham%20M.%22%2C%22lastName%22%3A%22Saleh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christopher%22%2C%22lastName%22%3A%22Cook%22%7D%5D%2C%22abstractNote%22%3A%22Anagen%20effluvium%20is%20a%20form%20of%20nonscarring%20alopecia%2C%20with%20two%20distinct%20types%20of%20anagen%20effluvium%5Cu2014dystrophic%20anagen%20effluvium%20and%20loose%20anagen%20syndrome.%5Cu00a0Dystrophic%20anagen%20effluvium%20is%20most%20commonly%20associated%20with%20chemotherapy%3B%20however%2C%20it%20can%20also%20manifest%20in%20cases%20of%20protein-energy%20deficiency%2C%20pemphigus%2C%20alopecia%20areata%2C%20and%20different%20forms%20of%20heavy%20metal%20poisoning.%20In%20this%20disorder%2C%20affected%20anagen%20hairs%20suffer%20a%20toxic%20or%20inflammatory%20insult%2C%20resulting%20in%20a%20hair%20shaft%20fracture.%5Cu00a0Loose%20anagen%20hair%20syndrome%20is%20an%20inherited%20condition%20characterized%20by%20loosely%20anchored%20anagen%20hairs%20that%20can%20be%20easily%20and%20painlessly%20pulled%20from%20the%20scalp.%5Cu00a0This%20condition%20arises%20due%20to%20hereditary%20keratin%20defects%20in%20the%20inner%20root%20sheath%2C%20the%20opposed%20companion%20layer%2C%20or%20both.%20The%20more%20commonly%20observed%20form%20of%20anagen%20effluvium%20is%20often%20called%20chemotherapy-induced%20alopecia%20due%20to%20its%20susceptibility%20to%20the%20effects%20of%20antimetabolites%2C%20alkylating%20drugs%2C%20and%20mitotic%20inhibitors%5Cu00a0used%20in%5Cu00a0chemotherapy.%5Cu00a0Hair%20shedding%20often%20occurs%20within%2014%20days%20of%20chemotherapy%20administration.%20Trichoscopy%20can%20reveal%20tapered%20fractures%20of%20anagen%20hairs%2C%20frequently%20resulting%20in%20hair%20shaft%20injury.%20In%20contrast%20to%20telogen%20effluvium%2C%20where%20the%20hairs%20are%20shed%2C%20the%20hairs%20in%20anagen%20effluvium%20are%20broken.%20Therefore%2C%20it%20might%20be%20argued%20that%20the%20term%20anagen%20effluvium%20is%20linguistically%20misleading%2C%20as%20effluvium%20refers%20to%20the%20act%20of%20shedding.%20Understandably%2C%20the%20hair%20loss%20associated%20with%20this%20disorder%20can%20be%20emotionally%20and%20psychologically%20distressing%20to%20the%20patient.%5Cu00a0The%20prognosis%20for%20a%20patient%20with%20anagen%20effluvium%20is%20guarded.%20No%20treatment%20has%20proven%20entirely%20effective%20in%20preventing%20or%20stopping%20hair%20loss%20in%5Cu00a0anagen%20effluvium.%20Patient%20education%20and%20aesthetic%20advice%20in%20managing%20hair%20loss%20are%20crucial.%20Expectations%20should%20be%20managed%20so%20that%20patients%20understand%20the%20unfortunate%20inevitability%20of%20the%20disorder%3B%20however%2C%20they%20should%20also%20be%20assured%20that%20most%20patients%20with%5Cu00a0anagen%20effluvium%20experience%20hair%20restoration%5Cu00a0following%5Cu00a0the%20completion%20of%20chemotherapy%2C%20although%20it%20often%20takes%20months%20or%20years%20before%20full%20recovery%20is%20attained.%20Unfortunately%2C%20hair%20thinning%20may%20persist%20in%20a%20few%20patients%20without%20complete%20recovery.%22%2C%22bookTitle%22%3A%22StatPearls%22%2C%22date%22%3A%222025%22%2C%22originalDate%22%3A%22%22%2C%22originalPublisher%22%3A%22%22%2C%22originalPlace%22%3A%22%22%2C%22format%22%3A%22%22%2C%22ISBN%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22ISSN%22%3A%22%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-17T16%3A23%3A10Z%22%7D%7D%2C%7B%22key%22%3A%22V9P3BUD5%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hac%5Cu0131necipo%5Cu011flu%20et%20al.%22%2C%22parsedDate%22%3A%222025-03-13%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHac%26%23x131%3Bnecipo%26%23x11F%3Blu%20F%2C%20%26%23xC7%3Belik%20G%2C%20Kartal%20SP.%20Anagen%20Effluvium%20in%20a%20Child%20Misusing%20Methotrexate%3A%20A%20Case%20Report%20With%20Dermoscopic%20Findings.%20Pediatr%20Dermatol.%202025%20Mar%2013%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Anagen%20Effluvium%20in%20a%20Child%20Misusing%20Methotrexate%3A%20A%20Case%20Report%20With%20Dermoscopic%20Findings%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fatmanur%22%2C%22lastName%22%3A%22Hac%5Cu0131necipo%5Cu011flu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G%5Cu00f6k%5Cu00e7en%22%2C%22lastName%22%3A%22%5Cu00c7elik%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Selda%20Pelin%22%2C%22lastName%22%3A%22Kartal%22%7D%5D%2C%22abstractNote%22%3A%22Anagen%20effluvium%20is%20a%20rare%20adverse%20effect%20of%20methotrexate%20therapy%2C%20generally%20associated%20with%20high-dose%20regimens.%20We%20report%20a%2012-year-old%20girl%20who%20developed%20abrupt%20hair%20loss%201%5Cu2009week%20after%20inadvertently%20taking%20methotrexate%2015%5Cu2009mg%20daily%20for%20five%20consecutive%20days%20%28total%2075%5Cu2009mg%29%2C%20without%20other%20signs%20of%20systemic%20toxicity.%20Trichoscopic%20examination%20and%20trichogram%20findings%20confirmed%20methotrexate-induced%20anagen%20effluvium%2C%20and%20spontaneous%20hair%20regrowth%20occurred%20after%202%5Cu2009months.%20This%20case%20underlines%20the%20importance%20of%20careful%20methotrexate%20dose%20monitoring%20and%20awareness%20that%20methotrexate%20toxicity%20can%20be%20associated%20with%20anagen%20effluvium%20even%20in%20the%20absence%20of%20other%20signs%20of%20toxicity.%22%2C%22date%22%3A%222025-03-13%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fpde.15927%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221525-1470%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22IQSBMDAQ%22%5D%2C%22dateModified%22%3A%222025-05-12T16%3A43%3A20Z%22%7D%7D%5D%7D 1.
Duvic M, Lemak NA, Valero V, Hymes SR, Farmer KL, Hortobagyi GN, et al. A randomized trial of minoxidil in chemotherapy-induced alopecia. J Am Acad Dermatol. 1996 July;35(1):74–8.
1.
Sharma PK, Gautam RK, Bhardwaj M, Kar HK. Isonicotinic acid hydrazide induced anagen effluvium and associated lichenoid eruption. J Dermatol. 2001 Dec;28(12):737–41.
1.
Yun SJ, Kim SJ. Hair loss pattern due to chemotherapy-induced anagen effluvium: a cross-sectional observation. Dermatology. 2007;215(1):36–40.
1.
Tallon B, Blanchard E, Goldberg LJ. Permanent chemotherapy-induced alopecia: case report and review of the literature. J Am Acad Dermatol. 2010 Aug;63(2):333–6.
1.
Yeager CE, Olsen EA. Treatment of chemotherapy-induced alopecia. Dermatol Ther. 2011;24(4):432–42.
1.
Curto-Barredo L, Segura S, Martín-Ezquerra G, Lloveras B, Gallardo F, Pujol RM. Anagen effluvium due to thallium poisoning derived from the intake of Chinese herbal medicine and rodenticide containing thallium salts. J Dermatol. 2015 Oct;42(10):1027–9.
1.
Bains A, Verma GK, Vedant D, Negi A. Anagen effluvium secondary to Gloriosa superba ingestion. Indian J Dermatol Venereol Leprol. 2016;82(6):677–80.
1.
Combalia A, Baliu-Piqué C, Fortea A, Ferrando J. Anagen Effluvium Following Acute Colchicine Poisoning. Int J Trichology. 2016;8(4):171–2.
1.
Campbell C, Bahrami S, Owen C. Anagen Effluvium Caused by Thallium Poisoning. JAMA Dermatol. 2016 June 1;152(6):724–6.
1.
Dunnill CJ, Al-Tameemi W, Collett A, Haslam IS, Georgopoulos NT. A Clinical and Biological Guide for Understanding Chemotherapy-Induced Alopecia and Its Prevention. Oncologist. 2018 Jan;23(1):84–96.
1.
Ghias MH, Amin BD, Kutner AJ. Albendazole-induced anagen effluvium. JAAD Case Rep. 2020 Jan;6(1):54–6.
1.
Sharma R, Poddar S, Podder I. Azathioprine Induced Anagen Effluvium- An Uncommon Adverse Effect of a Commonly Used Drug. Indian J Dermatol. 2022;67(6):815–7.
1.
Starace M, Orlando G, Bruni F, Alessandrini A, Piraccini BM. Anagen effluvium and the role of trichoscopy. Clin Exp Dermatol. 2022 Mar;47(3):589–91.
1.
Saleh D, Nassereddin A, Saleh HM, Cook C. Anagen Effluvium. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
1.
Hacınecipoğlu F, Çelik G, Kartal SP. Anagen Effluvium in a Child Misusing Methotrexate: A Case Report With Dermoscopic Findings. Pediatr Dermatol. 2025 Mar 13;