Androgenetic alopecia (AGA), commonly known as male or female pattern hair loss, is a well-recognized cause of hair loss in adults. However, it is an under-recognized cause of hair loss in children and adolescents. This article aims to shed light on the epidemiology, clinical features, associated diseases, and treatment response of AGA in the pediatric population.
AGA in children is not uncommon, but its incidence and prevalence are unknown. It is associated with a strong family history of AGA and can typically be diagnosed clinically by physical examination and trichoscopy. The average age of puberty has decreased by about three years during the past century in developed countries, attributed to improved nutrition and increased obesity rates, with increasing evidence that environmental endocrine disruptor chemicals may play a role. The shift of adrenarche and pubertal onset toward younger ages may be increasing the prevalence of pediatric AGA, as children are exposed to increased levels of circulating androgens at earlier ages, and AGA may develop earlier in genetically susceptible children.
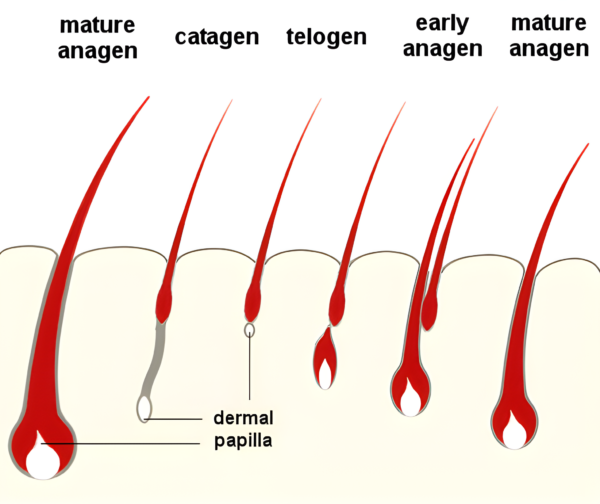
The clinical presentation of AGA in children is similar to that in adults, with thinning of the hair primarily on the top and front of the scalp. However, the pattern of hair loss can vary, and in some cases, children may exhibit a “Ludwig” pattern of hair loss, usually associated with female pattern hair loss. The diagnosis of AGA in children is primarily clinical, based on the pattern of hair loss and the presence of miniaturized hairs. Trichoscopy can be a useful tool in the diagnosis, showing increased hair shaft variability due to follicle miniaturization.
AGA in children can be associated with other signs of androgen excess, such as acne and hirsutism, and with abnormal pubertal development. In such cases, an endocrinologic evaluation should be considered. For example, hormonal testing in an 11-year-old boy with AGA and gynecomastia revealed late-onset congenital adrenal hyperplasia. Hair loss can have significant mental and social effects, and a psychological evaluation to determine the social and mental health effects should be considered.
There is no approved therapy for AGA in children. However, some therapeutic agents used in adults with AGA have also been used with some success in children. Topical (applied onto the scalp skin) minoxidil, although not approved for use on children, has been used under the supervision of dermatologists with some success. In a retrospective study, girls aged 11-18 years treated with topical minoxidil solution reported stabilization of hair loss at one year of use, and boys treated with topical minoxidil solution or foam reported cessation of hair loss or thicker hair density at follow-up, after at least six months. A larger report on minoxidil efficacy for AGA in children relied on data from a survey of clinicians who treated children seeking help for thinning hair. The results showed that 95% of the children treated with topical minoxidil solution for approximately 18 months showed improved scalp hair coverage or slowing of additional hair thinning.
Although topical minoxidil is generally well-tolerated in adults, caution should be used in children. There are reports of minoxidil overdose in children who accidentally ingest the product orally, causing dangerous hypotension and sinus tachycardia. Thus, if topical minoxidil is to be used in a young child, parents must be educated on the dangers if ingested orally and be instructed to keep the product in a location inaccessible to the child. Any diagnosis or treatment of hair loss in children should only be with the supervision of a fully qualified clinician.
In conclusion, AGA in children is not as rare as previously thought. Clinicians should be aware of this condition and be prepared to diagnose and manage it appropriately. The use of topical minoxidil, although not approved for use in children, has shown some results in the treatment of pediatric AGA. However, it is crucial to educate parents about the potential risks associated with its use, particularly the danger of oral ingestion. Further research is needed to better understand the epidemiology of AGA in children and to develop safe and effective treatments for this population.
Bibliography
11711645 {11711645:WZ6ADD4T},{11711645:S6FCWNBE},{11711645:SZFCSEPZ},{11711645:TA3DE55R},{11711645:33D7XWQK},{11711645:ESJ4V924},{11711645:HIGN6PFM} items 1 vancouver 0 date asc 134 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3A%22zotpress-b781de9cc6ed224aa63caff21de250f3%22%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22S6FCWNBE%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Tosti%20et%20al.%22%2C%22parsedDate%22%3A%222005-03%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3ETosti%20A%2C%20Iorizzo%20M%2C%20Piraccini%20BM.%20Androgenetic%20alopecia%20in%20children%3A%20report%20of%2020%20cases.%20Br%20J%20Dermatol.%202005%20Mar%3B152%283%29%3A556%26%23x2013%3B9.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Androgenetic%20alopecia%20in%20children%3A%20report%20of%2020%20cases%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Tosti%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Iorizzo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20M.%22%2C%22lastName%22%3A%22Piraccini%22%7D%5D%2C%22abstractNote%22%3A%22Androgenetic%20alopecia%20%28AGA%29%20is%20the%20most%20common%20type%20of%20hair%20loss%20in%20adults.%20Although%20there%20are%20differences%20in%20the%20age%20at%20onset%2C%20the%20disease%20starts%20after%20puberty%20when%20enough%20testosterone%20is%20available%20to%20be%20transformed%20into%20dihydrotestosterone.%20We%20report%2020%20prepubertal%20children%20with%20AGA%2C%2012%20girls%20and%20eight%20boys%2C%20age%20range%206-10%20years%2C%20observed%20over%20the%20last%204%20years.%20All%20had%20normal%20physical%20development.%20Clinical%20examination%20showed%20hair%20loss%20with%20thinning%20and%20widening%20of%20the%20central%20parting%20of%20the%20scalp%2C%20both%20in%20boys%20and%20girls.%20In%20eight%20cases%20frontal%20accentuation%20and%20breach%20of%20frontal%20hairline%20were%20also%20present.%20The%20clinical%20diagnosis%20was%20confirmed%20by%20pull%20test%2C%20trichogram%20and%20dermoscopy%20in%20all%20cases%2C%20and%20by%20scalp%20biopsy%20performed%20in%20six%20cases.%20There%20was%20a%20strong%20family%20history%20of%20AGA%20in%20all%20patients.%20The%20onset%20of%20AGA%20is%20not%20expected%20to%20be%20seen%20in%20prepubertal%20patients%20without%20abnormal%20androgen%20levels.%20A%20common%20feature%20observed%20in%20our%20series%20of%20children%20with%20AGA%20was%20a%20strong%20genetic%20predisposition%20to%20the%20disease.%20Although%20the%20pathogenesis%20remains%20speculative%2C%20endocrine%20evaluation%20and%20a%20strict%20follow-up%20are%20strongly%20recommended.%22%2C%22date%22%3A%222005-03%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1365-2133.2004.06279.x%22%2C%22ISSN%22%3A%220007-0963%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A15%3A19Z%22%7D%7D%2C%7B%22key%22%3A%22WZ6ADD4T%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Kim%20et%20al.%22%2C%22parsedDate%22%3A%222006-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EKim%20BJ%2C%20Kim%20JY%2C%20Eun%20HC%2C%20Kwon%20OS%2C%20Kim%20MN%2C%20Ro%20BI.%20Androgenetic%20alopecia%20in%20adolescents%3A%20a%20report%20of%2043%20cases.%20J%20Dermatol.%202006%20Oct%3B33%2810%29%3A696%26%23x2013%3B9.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Androgenetic%20alopecia%20in%20adolescents%3A%20a%20report%20of%2043%20cases%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Beom%20Joon%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ji%20Young%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hee%20Chul%22%2C%22lastName%22%3A%22Eun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Oh%20Sang%22%2C%22lastName%22%3A%22Kwon%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Myeung%20Nam%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Byung%20In%22%2C%22lastName%22%3A%22Ro%22%7D%5D%2C%22abstractNote%22%3A%22Androgenetic%20alopecia%20%28AGA%29%20is%20the%20most%20common%20type%20of%20hair%20loss%20in%20adults%2C%20but%20it%20also%20occurs%20in%20adolescents%2C%20though%20its%20prevalence%20among%20this%20younger%20population%20is%20not%20well%20established.%20The%20purpose%20of%20this%20study%20was%20to%20evaluate%20the%20clinical%20manifestations%20and%20endocrine%20status%20of%20adolescent%20patients%20with%20AGA%20in%20Korea.%20This%205-year%20%28January%202001-August%202005%29%20clinical%20study%20involved%2043%20adolescent%20patients%20with%20AGA.%20Testosterone%20and%20dehydroepiandrosterone%20sulfate%20%28DHEA-S%29%20laboratory%20studies%20were%20undertaken%20to%20investigate%20androgenic%20hormonal%20effects.%20Hair%20loss%20severity%20was%20categorized%20using%20the%20Hamilton-Norwood%20and%20Ludwig%20classifications.%20Gender%20ratio%20showed%20a%20male%20predominance%20%28M%20%3A%20F%2C%2035%3A8%29%2C%20and%20a%20mean%20age%20at%20onset%20of%2016.8%20years.%20These%20adolescent%20patients%20showed%20milder%20symptoms%20than%20adults%2C%20and%20a%20family%20history%20of%20alopecia%20was%20found%20in%2072.1%25%2C%20which%20is%20greater%20than%20that%20reported%20in%20adults%2C%20which%20ranges%2030.9-64.5%25.%20Seborrheic%20dermatitis%20%2827.9%25%29%20was%20the%20condition%20most%20commonly%20associated%20with%20AGA%20among%20our%20study%20subjects%2C%20followed%20in%20descending%20order%20by%20acne%20vulgaris%20and%20atopic%20dermatitis.%20Serum%20levels%20of%20testosterone%20and%20DHEA-S%20were%20within%20normal%20limits%2C%20except%20in%20one%20subject.%20Our%20study%20shows%20the%20clinical%20characteristics%20of%20AGA%20in%20Korean%20adolescents.%22%2C%22date%22%3A%222006-10%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1346-8138.2006.00161.x%22%2C%22ISSN%22%3A%220385-2407%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A14%3A49Z%22%7D%7D%2C%7B%22key%22%3A%22TA3DE55R%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Vozza%20et%20al.%22%2C%22parsedDate%22%3A%222012%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EVozza%20A%2C%20Piccolo%20V%2C%20Russo%20T%2C%20Vozza%20G.%20Familial%20androgenetic%20alopecia%20in%20siblings%20with%20normal%20endocrinological%20status.%20Pediatr%20Dermatol.%202012%3B29%284%29%3A534%26%23x2013%3B5.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Familial%20androgenetic%20alopecia%20in%20siblings%20with%20normal%20endocrinological%20status%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Antonio%22%2C%22lastName%22%3A%22Vozza%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vincenzo%22%2C%22lastName%22%3A%22Piccolo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Teresa%22%2C%22lastName%22%3A%22Russo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Giuseppe%22%2C%22lastName%22%3A%22Vozza%22%7D%5D%2C%22abstractNote%22%3A%22Androgenetic%20alopecia%20%28AGA%29%20is%20the%20most%20common%20type%20of%20hair%20loss%20in%20adults%2C%20but%20it%20has%20been%20rarely%20reported%20in%20children.%20We%20report%20two%20cases%20of%20AGA%20in%20two%20siblings%2C%20aged%206%20and%208%2C%20whose%20mother%20had%20the%20same%20condition%2C%20without%20any%20association%20with%20other%20skin%20diseases%20or%20abnormalities%20in%20endocrinologic%20examinations.%22%2C%22date%22%3A%222012%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1525-1470.2011.01528.x%22%2C%22ISSN%22%3A%221525-1470%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A14%3A36Z%22%7D%7D%2C%7B%22key%22%3A%22HIGN6PFM%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rossi%20et%20al.%22%2C%22parsedDate%22%3A%222019-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3ERossi%20A%2C%20D%26%23x2019%3BArino%20A%2C%20Pigliacelli%20F%2C%20Caro%20G%2C%20Muscianese%20M%2C%20Fortuna%20MC%2C%20et%20al.%20The%20diagnosis%20of%20androgenetic%20alopecia%20in%20children%3A%20Considerations%20of%20pathophysiological%20plausibility.%20Australas%20J%20Dermatol.%202019%20Nov%3B60%284%29%3Ae279%26%23x2013%3B83.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20diagnosis%20of%20androgenetic%20alopecia%20in%20children%3A%20Considerations%20of%20pathophysiological%20plausibility%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alfredo%22%2C%22lastName%22%3A%22Rossi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrea%22%2C%22lastName%22%3A%22D%27Arino%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Flavia%22%2C%22lastName%22%3A%22Pigliacelli%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gemma%22%2C%22lastName%22%3A%22Caro%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marta%22%2C%22lastName%22%3A%22Muscianese%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%20Caterina%22%2C%22lastName%22%3A%22Fortuna%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marta%22%2C%22lastName%22%3A%22Carlesimo%22%7D%5D%2C%22abstractNote%22%3A%22Androgenetic%20alopecia%20%28AGA%29%2C%20one%20of%20the%20most%20common%20causes%20of%20hair%20loss%20in%20men%20and%20women%2C%20is%20an%20infrequent%20cause%20of%20alopecia%20in%20children.%20In%20AGA%2C%20patients%20generally%20start%20noticing%20hair%20thinning%20after%20the%20onset%20of%20puberty%20due%20to%20progressive%20miniaturisation%20of%20the%20hair%20follicle%20which%20leads%20to%20vellus%20transformation%20of%20terminal%20hair.%20However%2C%20the%20occurrence%20of%20prepubertal%20AGA%20has%20rarely%20been%20reported%20in%20the%20literature.%20The%20pathophysiology%20of%20AGA%20is%20tightly%20linked%20to%20androgen%20hormones%3B%20prepubertal%20children%20do%20not%20usually%20produce%20significant%20amounts%20of%20adrenal%20or%20gonadal%20androgens.%20When%20it%20does%20occur%2C%20an%20underlying%20abnormality%20should%20be%20suspected.%20Secondary%20causes%20of%20AGA%20must%20be%20excluded%20when%20evaluating%20a%20patient%20before%20the%20appearance%20of%20puberty.%20Premature%20puberty%2C%20polycystic%20ovarian%20syndrome%20and%20other%20causes%20of%20hyperandrogenism%20can%20present%20with%20hair%20loss%20in%20an%20androgenetic%20pattern.%20This%20article%20reviews%20the%20normal%20physiology%20of%20androgen%20hormones%20and%20their%20role%20in%20the%20pathophysiology%20of%20childhood%20AGA.%22%2C%22date%22%3A%222019-11%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fajd.13079%22%2C%22ISSN%22%3A%221440-0960%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A14%3A08Z%22%7D%7D%2C%7B%22key%22%3A%22SZFCSEPZ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Griggs%20et%20al.%22%2C%22parsedDate%22%3A%222021-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EGriggs%20J%2C%20Burroway%20B%2C%20Tosti%20A.%20Pediatric%20androgenetic%20alopecia%3A%20A%20review.%20J%20Am%20Acad%20Dermatol.%202021%20Nov%3B85%285%29%3A1267%26%23x2013%3B73.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Pediatric%20androgenetic%20alopecia%3A%20A%20review%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jacob%22%2C%22lastName%22%3A%22Griggs%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Brandon%22%2C%22lastName%22%3A%22Burroway%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Antonella%22%2C%22lastName%22%3A%22Tosti%22%7D%5D%2C%22abstractNote%22%3A%22OBJECTIVES%3A%20Androgenetic%20alopecia%20%28AGA%29%20is%20a%20well-known%20cause%20of%20hair%20loss%20in%20adults%20but%20is%20an%20under-recognized%20cause%20of%20hair%20loss%20in%20children%20and%20adolescents.%20We%20reviewed%20the%20existing%20literature%20regarding%20androgenetic%20alopecia%20in%20the%20pediatric%5C%2Fadolescent%20population.%5CnMETHODS%3A%20PubMed%20searches%20were%20performed%20to%20identify%20all%20articles%20discussing%20AGA%20in%20a%20pediatric%5C%2Fadolescent%20population%20published%20up%20to%20December%202018.%5CnRESULTS%3A%20We%20identified%207%20articles%20discussing%20androgenetic%20alopecia%20in%20patients%20aged%20younger%20than%2018.%20One%20of%20these%20articles%20was%20a%20review%20containing%20data%20from%203%20conference%20abstracts%2C%20which%20were%20also%20included%20in%20the%20analysis.%20A%20total%20of%20655%20cases%20of%20androgenetic%20alopecia%20were%20found.%5CnLIMITATIONS%3A%20Data%20are%20limited%20to%20retrospective%20reviews%20and%20case%20reports%5C%2Fseries.%5CnCONCLUSION%3A%20AGA%20in%20the%20pediatric%20population%20is%20not%20uncommon%2C%20but%20its%20incidence%20and%20prevalence%20are%20unknown.%20It%20is%20associated%20with%20a%20strong%20family%20history%20of%20AGA%20and%20can%20typically%20be%20diagnosed%20clinically%20by%20physical%20examination%20and%20trichoscopy.%20Topical%20minoxidil%2C%20although%20not%20approved%2C%20has%20been%20used%20with%5Cu00a0success.%20Other%20treatment%20modalities%20are%20poorly%20studied%20in%20children.%22%2C%22date%22%3A%222021-11%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2019.08.018%22%2C%22ISSN%22%3A%221097-6787%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A13%3A50Z%22%7D%7D%2C%7B%22key%22%3A%2233D7XWQK%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22%5Cu00d6zcan%22%2C%22parsedDate%22%3A%222022%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3E%26%23xD6%3Bzcan%20D.%20Pediatric%20androgenetic%20alopecia%3A%20a%20retrospective%20review%20of%20clinical%20characteristics%2C%20hormonal%20assays%20and%20metabolic%20syndrome%20risk%20factors%20in%2023%20patients.%20An%20Bras%20Dermatol.%202022%3B97%282%29%3A166%26%23x2013%3B72.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Pediatric%20androgenetic%20alopecia%3A%20a%20retrospective%20review%20of%20clinical%20characteristics%2C%20hormonal%20assays%20and%20metabolic%20syndrome%20risk%20factors%20in%2023%20patients%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Deren%22%2C%22lastName%22%3A%22%5Cu00d6zcan%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Androgenetic%20alopecia%20in%20the%20pediatric%20population%20is%20rarely%20discussed%20in%20the%20literature.%20Although%20the%20prevalence%20of%20the%20metabolic%20syndrome%20is%20increased%20in%20patients%20with%20early-onset%20androgenetic%20alopecia%2C%20the%20presence%20of%20metabolic%20syndrome%20risk%20factors%20in%20pediatric%20androgenetic%20alopecia%20is%20unknown.%5CnOBJECTIVE%3A%20To%20evaluate%20the%20demographics%2C%20medical%20and%20family%20histories%2C%20clinical%20and%20trichoscopic%20features%2C%20androgenic%20hormones%2C%20and%20metabolic%20syndrome%20risk%20factors%20in%20pediatric%20androgenetic%20alopecia.%5CnMETHODS%3A%20The%20medical%20reports%20of%20pediatric%20patients%20with%20androgenetic%20alopecia%20were%20reviewed.%5CnRESULTS%3A%20The%20study%20included%2023%20patients%20%2812%20females%20and%2011%20males%29%20with%20a%20mean%20age%20of%2015%2C3%5Cu202f%5Cu00b1%5Cu202f2%2C1%20years.%20Sixteen%20patients%20had%20adolescent%20androgenetic%20alopecia%20and%20seven%2C%20had%20childhood%20alopecia.%20Nine%20patients%20reported%20a%20family%20history%2C%20all%20of%20whom%20had%20adolescent%20androgenetic%20alopecia.%20Hyperandrogenism%20was%20noted%20in%20three%20patients%20with%20adolescent%20androgenetic%20alopecia.%20The%20most%20common%20hair%20loss%20pattern%20was%20diffuse%20thinning%20at%20the%20crown%20with%20preservation%20of%20the%20frontal%20hairline%20which%20was%20noted%20in%2010%20patients%20%2843.5%25%29%2C%20six%20of%20whom%20were%20males.%20Fourteen%20patients%20%2860.9%25%29%20had%20at%20least%20one%20metabolic%20syndrome%20risk%20factor.%20The%20most%20common%20risk%20factor%20was%20obesity%20or%20overweight%20%2847.8%25%29%20followed%20by%20insulin%20resistance%20%2821.7%25%29%2C%20high%20fasting%20blood%20glucose%20%2813%25%29%2C%20high%20blood%20pressure%20%284.4%25%29%20and%20lipid%20abnormalities%20%284.4%25%29.%5CnSTUDY%20LIMITATIONS%3A%20Retrospective%20study%3B%20lack%20of%20a%20control%20group.%5CnCONCLUSION%3A%20Pediatric%20androgenetic%20alopecia%20is%20often%20associated%20with%20metabolic%20syndrome%20risk%20factors.%20Therefore%2C%20androgenetic%20alopecia%20in%20the%20pediatric%20population%20may%20indicate%20a%20future%20metabolic%20syndrome%20which%20warrants%20an%20accurate%20and%20prompt%20diagnosis%20for%20early%20screening%20and%20treatment.%22%2C%22date%22%3A%222022%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.abd.2021.06.006%22%2C%22ISSN%22%3A%221806-4841%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A13%3A31Z%22%7D%7D%2C%7B%22key%22%3A%22ESJ4V924%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Gomes%20and%20Soares%22%2C%22parsedDate%22%3A%222023-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EGomes%20TF%2C%20Soares%20RO.%20Pediatric%20androgenetic%20alopecia%3A%20an%20updated%20review.%20J%20Dtsch%20Dermatol%20Ges.%202023%20Jan%3B21%281%29%3A19%26%23x2013%3B25.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Pediatric%20androgenetic%20alopecia%3A%20an%20updated%20review%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tiago%20Fernandes%22%2C%22lastName%22%3A%22Gomes%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rui%20Oliveira%22%2C%22lastName%22%3A%22Soares%22%7D%5D%2C%22abstractNote%22%3A%22Pediatric%20androgenetic%20alopecia%20is%20an%20underrecognized%20disorder.%20A%20clinical%20evaluation%20with%20trichoscopy%20should%20be%20made%20in%20children%20and%20adolescents%20with%20hair%20loss%20and%5C%2For%20reduced%20hair%20density.%20Diagnosis%20is%20usually%20clinical%2C%20by%20observation%20of%20the%20hair%20loss%20pattern%20and%20performance%20of%20trichoscopy.%20In%20some%20cases%2C%20hyperandrogenism%20should%20be%20excluded.%20Although%20there%20is%20no%20approved%20therapy%20for%20androgenetic%20alopecia%20in%20pediatric%20age%2C%20topical%20minoxidil%2C%20oral%20minoxidil%20and%20topical%20finasteride%20may%20be%20very%20useful.%20Hair%20transplant%20may%20be%20an%20option%20for%20girls%20in%20selected%20cases.%20This%20article%20is%20a%20review%20of%20the%20current%20state%20of%20evidence%20concerning%20pediatric%20androgenetic%20alopecia.%22%2C%22date%22%3A%222023-01%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fddg.14940%22%2C%22ISSN%22%3A%221610-0387%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22RZEC4FR5%22%5D%2C%22dateModified%22%3A%222023-05-20T16%3A16%3A07Z%22%7D%7D%5D%7D 1.
Tosti A, Iorizzo M, Piraccini BM. Androgenetic alopecia in children: report of 20 cases. Br J Dermatol. 2005 Mar;152(3):556–9.
1.
Kim BJ, Kim JY, Eun HC, Kwon OS, Kim MN, Ro BI. Androgenetic alopecia in adolescents: a report of 43 cases. J Dermatol. 2006 Oct;33(10):696–9.
1.
Vozza A, Piccolo V, Russo T, Vozza G. Familial androgenetic alopecia in siblings with normal endocrinological status. Pediatr Dermatol. 2012;29(4):534–5.
1.
Rossi A, D’Arino A, Pigliacelli F, Caro G, Muscianese M, Fortuna MC, et al. The diagnosis of androgenetic alopecia in children: Considerations of pathophysiological plausibility. Australas J Dermatol. 2019 Nov;60(4):e279–83.
1.
Griggs J, Burroway B, Tosti A. Pediatric androgenetic alopecia: A review. J Am Acad Dermatol. 2021 Nov;85(5):1267–73.
1.
Özcan D. Pediatric androgenetic alopecia: a retrospective review of clinical characteristics, hormonal assays and metabolic syndrome risk factors in 23 patients. An Bras Dermatol. 2022;97(2):166–72.
1.
Gomes TF, Soares RO. Pediatric androgenetic alopecia: an updated review. J Dtsch Dermatol Ges. 2023 Jan;21(1):19–25.