Introduction: Eosinophilic folliculitis (EF) is an inflammatory dermatosis characterized by recurrent, intensely pruritic papules and pustules centered on hair follicles, accompanied histologically by prominent eosinophil infiltration. First described in the 1970s among otherwise healthy individuals, EF later gained prominence as a cutaneous marker of immunosuppression, particularly in persons with human immunodeficiency virus (HIV) infection. However, EF may also arise in association with hematologic malignancies, after bone marrow transplantation, in patients receiving certain medications, or idiopathically in immunocompetent hosts. Though often chronic and relapsing, EF is not life–threatening; its primary burden lies in relentless itching, potential scarring, and diminished quality of life. This article provides an exploration of EF: its epidemiology, pathogenesis, clinical features, diagnostic approach, management strategies and prognostic considerations.
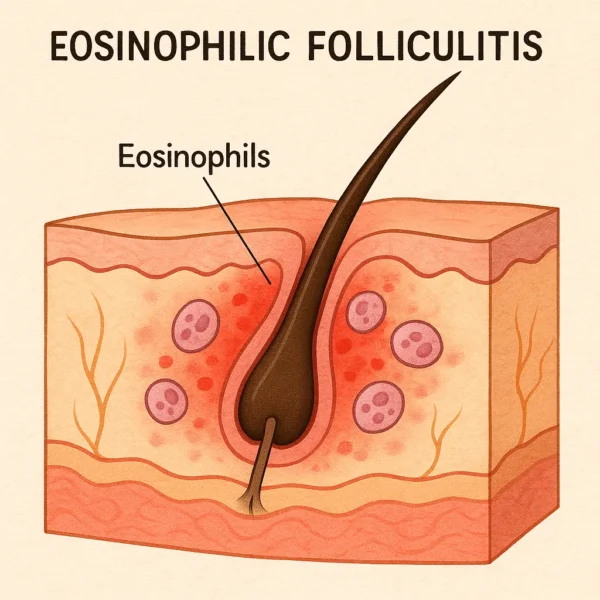
Anatomy and Pathophysiology of Eosinophilic Folliculitis: The pilosebaceous unit comprises a hair follicle, its associated sebaceous gland, the arrector pili muscle and the surrounding sheath. Eosinophilic folliculitis involves inflammation predominantly at the level of the follicular infundibulum, where keratinocytes, sebum and hair shafts converge. In EF, an aberrant immune response, mediated by type 2 helper T (Th2) lymphocytes, leads to recruitment of eosinophils into the follicular space and adjacent dermis. Activated eosinophils release cytotoxic granule proteins (e.g., major basic protein, eosinophil peroxidase), cytokines (e.g., interleukin-5) and lipid mediators, which disrupt follicular structure, provoke tissue edema, and produce intense pruritus.
Although the precise inciting antigen remains unknown, several mechanisms have been proposed:
Hypersensitivity to cutaneous flora : Reaction to resident microorganisms (e.g., Malassezia yeasts or Demodex mites) within follicles.Drug–induced : Certain medications, particularly chemotherapy agents and highly active antiretroviral therapy (HAART), may dysregulate cytokine networks, promoting eosinophilia.Underlying immunosuppression : In HIV-infected patients, Th2 skewing and diminished CD4+ T cell surveillance permit aberrant eosinophilic responses. Epidemiology and Risk Factors: EF can be broadly classified into four clinical subtypes:
Classic (Ofuji) disease : Occurs in otherwise healthy adults, originally described in Japanese patients; may exhibit seasonal exacerbations.HIV–associated EF : Emerged in the pre-HAART era as a cutaneous manifestation in patients with advanced immunodeficiency (CD4+ counts often <300 cells/µL).Hematologic–malignancy–associated EF : Reported in individuals with leukemia, lymphoma or after bone marrow transplantation.Drug–related EF : Linked to medications such as carbamazepine, all-trans retinoic acid, and indinavir. Although classic EF exhibits no strong sex predilection, HIV-associated EF disproportionately affects male patients, reflecting the demographics of the epidemic. Onset typically occurs in the third to fifth decades of life. Seasonal variation, worsening in spring and summer, suggests a role for ultraviolet light exposure and heat in precipitating flares.
Clinical Presentation: EF presents as recurrent crops of pruritic, folliculocentric lesions most prominent on the face, scalp, upper trunk and extensor surfaces of the limbs. Key features include:
Lesion morphology : Erythematous papules, papulopustules or small nodules (2–5 mm) centered on hair follicles. Lesions may coalesce into arcuate or annular plaques.Distribution : Predilection for seborrheic and sun–exposed areas; cheeks, frontal and temporal scalp, upper back and chest.Pruritus : Often severe and may intensify at night or in warm environments, leading to excoriations and potential secondary infection.Chronicity : EF tends to follow a relapsing–remitting course, with flares lasting weeks to months, interspersed with periods of relative quiescence. In HIV-associated EF, lesions may be more widespread and refractory to therapy. Systemic symptoms (e.g., fever, malaise) are uncommon but may appear in drug–induced cases.
Differential Diagnosis: EF must be distinguished from other papulopustular and follicular disorders:
Bacterial folliculitis : Staphylococcus aureus –driven pustules; often responsive to antibiotics.Malassezia (Pityrosporum) folliculitis : Pruritic monomorphic papules and pustules on trunk; KOH preparation reveals yeasts.Demodex folliculitis (Demodicosis) : Associated with mite overgrowth; diagnosed by standardized skin surface biopsy.Acne vulgaris : Comedones, inflammatory papules and cysts; absence of eosinophilia.Papular urticaria : Hypersensitivity to insect bites; intensely pruritic papules with central punctum. Accurate differentiation hinges on history, lesion distribution, associated risk factors and histopathology.
Diagnostic Work-up: The cornerstone of EF diagnosis is skin biopsy of a representative lesion. Histopathologic hallmarks include:
Folliculocentric mixed inflammatory infiltrate : Predominantly eosinophils within the infundibular lumen and perifollicular dermis.Spongiosis and microabscess formation : Occasional eosinophilic pustules within follicular epithelium.Variable mucin deposition : May be seen in chronic lesions.Absence of fungal or bacterial organisms : Special stains (PAS, Gram) and microbiological cultures are negative. Laboratory evaluation may reveal peripheral eosinophilia, especially in classic and drug-related EF, but this is neither sensitive nor specific. In HIV-associated cases, assessment of CD4+ count and viral load can guide overall care but the data cannot be used to confirm EF.
Management Strategies: Therapy for EF aims to alleviate pruritus, reduce lesion burden and prevent recurrences. Treatment must be tailored to the clinical subtype, disease severity and patient comorbidities.
Topical Therapies: Corticosteroids : Mid- to high-potency topical corticosteroids applied once or twice daily often yield rapid improvement. Calcineurin inhibitors : Topical tacrolimus or pimecrolimus provides steroid-sparing alternatives, particularly for facial lesions or long-term maintenance. Keratolytics : Agents such as salicylic acid or urea creams may enhance follicular penetration of anti-inflammatory drugs.Systemic Therapies: Oral indomethacin ; among the most consistently effective systemic agents in classic and HIV-associated EF. Mechanism involves inhibition of eosinophil chemotaxis and prostaglandin synthesis. Oral corticosteroids ; reserved for severe flares due to adverse effect profile. Isotretinoin ; beneficial in refractory cases by reducing follicular keratinization and sebum production. Antihistamines ; First-generation H1-antagonists (e.g., hydroxyzine) for symptomatic pruritus relief. Other agents; Dapsone, colchicine and phototherapy (UVA1 or narrowband UVB) have demonstrated efficacy in select case series.HIV-Associated EF: Antiretroviral therapy : Immune reconstitution via HAART frequently ameliorates EF lesions; rises in CD4+ count correlate with clinical improvement. Concurrent EF therapy : Indomethacin or topical steroids may be employed until immune recovery ensues.Drug-Induced EF: Drug cessation or substitution : Discontinuation of the offending agent is paramount. Symptomatic treatment : Short courses of topical or systemic anti-inflammatories during washout. Prognosis and Follow-Up: EF is typically chronic and relapsing. Without appropriate therapy, lesions may persist for months to years, waxing and waning with environmental triggers (e.g., heat, ultraviolet exposure). Key prognostic considerations include:
Subtype : Classic EF may remit spontaneously, whereas HIV-associated and hematologic-malignancy-associated EF often require long-term management.Treatment adherence : Regular use of topical agents and compliance with systemic regimens reduce recurrence.Immune status : Restoration of immune competence favors resolution, whether via HAART in HIV or recovery from chemotherapy. Periodic dermatologic evaluation every 3–6 months is advisable to monitor disease activity, adjust therapy and screen for treatment side effects.
Prevention and Patient Education: Although no measures can entirely prevent EF, patients can minimize flares and discomfort through:
Skincare routines : Gentle cleansing, avoidance of abrasive scrubs and selection of noncomedogenic moisturizers.Sun protection : Broad-spectrum sunscreens and physical barriers to reduce ultraviolet-induced exacerbations.Temperature and humidity control : Air conditioning or fans to mitigate heat and sweating.Stress management : Psychological stress may worsen pruritus and inflammation.Medication review : Periodic reassessment of drug regimens to identify potential culprits in drug-related EF. Clear communication regarding the chronic nature of EF and its treatment objectives, symptom control rather than cure, helps set realistic expectations and fosters adherence.
Future Directions: Emerging insights into the molecular drivers of EF may yield novel targeted therapies. Potential avenues include:
Biologics : Agents targeting interleukin-5 or eosinophil receptors (e.g., mepolizumab) offer promise in eosinophil-mediated diseases but remain untested in EF.JAK inhibitors : By interrupting cytokine signaling pathways, these drugs may attenuate Th2-driven inflammation.Microbiome modulation : As interactions with cutaneous flora may contribute to EF pathogenesis, probiotics or antimicrobial peptides could emerge as adjuncts. Rigorous clinical trials are needed to establish safety, efficacy and optimal dosing regimens for these novel modalities.
Conclusion: Eosinophilic folliculitis represents a distinctive follicular dermatitis marked by intense pruritus, eosinophil-rich inflammation and a chronic relapsing course. Its occurrence across diverse clinical settings, from immunocompetent adults to profoundly immunosuppressed patients, emphasizes the multifactorial underpinnings of EF. Accurate diagnosis hinges on clinicopathologic correlation, while effective management requires a personalized combination of topical and systemic therapies tailored to disease subtype and severity. Although EF remains incurable, most patients achieve substantial relief with appropriate interventions and supportive measures. Ongoing research into the immunologic and microbial triggers of EF holds promise for more precise, durable treatments in the years ahead.
Bibliography
11711645 {11711645:C3MT4L4A},{11711645:3JCALIA6},{11711645:R4UM39IK},{11711645:L8TYBGLZ},{11711645:77CIHPQY},{11711645:WWD9TR2T},{11711645:2PZCLNCK},{11711645:PLNKDXAY},{11711645:QKB85JB8},{11711645:629IMP68},{11711645:BZJAB3VV},{11711645:NFG7JJ3E},{11711645:IFPEYTSL},{11711645:7HW9IZ2J},{11711645:B7IUMP5G},{11711645:PLVX28NU},{11711645:ULEUQ44U},{11711645:8DV29PBN},{11711645:BD4ULV3R} 1 vancouver 50 date asc 1819 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22PLNKDXAY%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ofuji%20et%20al.%22%2C%22parsedDate%22%3A%221970%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BOfuji%20S%2C%20Ogino%20A%2C%20Horio%20T%2C%20Oseko%20T%2C%20Uehara%20M.%20Eosinophilic%20pustular%20folliculitis.%20Acta%20Derm%20Venereol.%201970%3B50%283%29%3A195%26%23x2013%3B203.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20pustular%20folliculitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22Ofuji%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Ogino%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Horio%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Oseko%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Uehara%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221970%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220001-5555%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A55%3A53Z%22%7D%7D%2C%7B%22key%22%3A%22WWD9TR2T%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ishibashi%20et%20al.%22%2C%22parsedDate%22%3A%221974%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BIshibashi%20A%2C%20Nishiyama%20Y%2C%20Miyata%20C%2C%20Chujo%20T.%20Eosinophilic%20pustular%20folliculitis%20%28ofuji%29.%20Dermatologica.%201974%3B149%284%29%3A240%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28ofuji%29%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Ishibashi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Y.%22%2C%22lastName%22%3A%22Nishiyama%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Miyata%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%22%2C%22lastName%22%3A%22Chujo%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221974%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220011-9075%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A56%3A19Z%22%7D%7D%2C%7B%22key%22%3A%228DV29PBN%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Nervi%20et%20al.%22%2C%22parsedDate%22%3A%222006-08%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BNervi%20SJ%2C%20Schwartz%20RA%2C%20Dmochowski%20M.%20Eosinophilic%20pustular%20folliculitis%3A%20a%2040%20year%20retrospect.%20J%20Am%20Acad%20Dermatol.%202006%20Aug%3B55%282%29%3A285%26%23x2013%3B9.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20pustular%20folliculitis%3A%20a%2040%20year%20retrospect%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stephen%20J.%22%2C%22lastName%22%3A%22Nervi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Robert%20A.%22%2C%22lastName%22%3A%22Schwartz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marian%22%2C%22lastName%22%3A%22Dmochowski%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20is%20a%20noninfectious%20eosinophilic%20infiltration%20of%20hair%20follicles%20first%20described%2040%20years%20ago.%20There%20are%203%20variants%3A%20classic%20EPF%2C%20immunosuppression-associated%20%28mostly%20HIV-related%29%2C%20and%20infancy-associated%20EPF.%20EPF%20has%20been%20classified%20as%20an%20AIDS-defining%20illness.%20In%20both%20children%20and%20adults%20EPF%20should%20be%20viewed%20as%20a%20possible%20cutaneous%20sign%20of%20immunosuppression.%20However%2C%20it%20may%20also%20be%20seen%20in%20persons%20with%20normal%20immune%20status.%20We%20review%20EPF%20on%20the%2040th%20anniversary%20of%20its%20original%20description.%22%2C%22date%22%3A%222006-08%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2006.02.034%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A53%3A29Z%22%7D%7D%2C%7B%22key%22%3A%22L8TYBGLZ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Sufyan%20et%20al.%22%2C%22parsedDate%22%3A%222007-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSufyan%20W%2C%20Tan%20KB%2C%20Wong%20ST%2C%20Lee%20YS.%20Eosinophilic%20pustular%20folliculitis.%20Arch%20Pathol%20Lab%20Med.%202007%20Oct%3B131%2810%29%3A1598%26%23x2013%3B601.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20pustular%20folliculitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wajiha%22%2C%22lastName%22%3A%22Sufyan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kong-Bing%22%2C%22lastName%22%3A%22Tan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Soon-Tee%22%2C%22lastName%22%3A%22Wong%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yoke-Sun%22%2C%22lastName%22%3A%22Lee%22%7D%5D%2C%22abstractNote%22%3A%22Classical%20eosinophilic%20pustular%20folliculitis%2C%20or%20Ofuji%26%23039%3Bs%20disease%2C%20is%20a%20chronic%20and%20relapsing%20dermatosis%20that%20is%20predominantly%20reported%20in%20East%20Asian%20populations.%20Clinically%2C%20the%20disease%20typically%20begins%20as%20small%20papules%2C%20which%20enlarge%20and%20coalesce%20into%20a%20large%20plaque%2C%20usually%20on%20the%20face.%20The%20histopathology%20is%20characterized%20by%20a%20prominent%20eosinophilic%20infiltrate%20in%20the%20dermis%20with%20concentration%20around%20pilosebaceous%20units%2C%20often%20with%20eosinophilic%20microabscess%20formation.%20The%20differentiation%20of%20eosinophilic%20pustular%20folliculitis%20from%20other%20eosinophilic%20dermatoses%20is%20practically%20challenging%20and%20requires%20close%20clinicopathologic%20correlation.%20Eosinophilic%20pustular%20folliculitis%20may%20also%20be%20associated%20with%20human%20immunodeficiency%20virus%20infection%2C%20various%20drugs%2C%20and%20some%20lymphomas%20and%20could%20also%20be%20thought%20of%20as%20a%20nonspecific%20dermatopathologic%20pattern%20in%20such%20settings.%20The%20cause%20of%20classical%20eosinophilic%20pustular%20folliculitis%20is%20unknown%2C%20although%20immune%20processes%20are%20almost%20certain%20to%20play%20a%20key%20role%20in%20its%20pathogenesis.%22%2C%22date%22%3A%222007-10%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.5858%5C%2F2007-131-1598-EPF%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221543-2165%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A56%3A47Z%22%7D%7D%2C%7B%22key%22%3A%22C3MT4L4A%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Fujiyama%20and%20Tokura%22%2C%22parsedDate%22%3A%222013-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFujiyama%20T%2C%20Tokura%20Y.%20Clinical%20and%20histopathological%20differential%20diagnosis%20of%20eosinophilic%20pustular%20folliculitis.%20J%20Dermatol.%202013%20June%3B40%286%29%3A419%26%23x2013%3B23.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Clinical%20and%20histopathological%20differential%20diagnosis%20of%20eosinophilic%20pustular%20folliculitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Toshiharu%22%2C%22lastName%22%3A%22Fujiyama%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yoshiki%22%2C%22lastName%22%3A%22Tokura%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20is%20an%20inflammatory%20disease%20characterized%20by%20repeated%20pruritic%20follicular%20papules%20and%20pustules%20arranged%20in%20arcuate%20plaques%2C%20and%20folliculotropic%20infiltration%20of%20eosinophils.%20The%20diagnosis%20of%20EPF%20is%20occasionally%20difficult%20and%20problematic%20because%20EPF%20may%20share%20the%20clinical%20appearance%20and%20histological%20findings%20with%20other%20diseases.%20Moreover%2C%20EPF%20has%20several%20clinical%20subtypes%2C%20including%20the%20classical%20type%2C%20infantile%20type%20and%20immunosuppression-associated%20type.%20Because%20the%20therapies%20of%20EPF%20are%20relatively%20specific%20as%20compared%20to%20eczematous%20disorders%2C%20accurate%20diagnosis%20is%20essential%20for%20the%20management%20of%20EPF.%20Clinical%20differential%20diagnoses%20include%20tinea%2C%20acne%2C%20rosacea%2C%20eczematous%20dermatitis%2C%20granuloma%20faciale%2C%20autoimmune%20annular%20erythema%2C%20infestations%20and%20pustular%20dermatosis.%20Histologically%2C%20cutaneous%20diseases%20with%20eosinophilic%20infiltrates%20can%20be%20differentially%20diagnosed.%20Follicular%20mucinosis%2C%20mycosis%20fungoides%20and%20other%20cutaneous%20T-cell%20lymphomas%20are%20the%20most%20important%20differential%20diagnoses%20both%20clinically%20and%20histopathologically.%20It%20should%20be%20kept%20in%20mind%20particularly%20that%20the%20initial%20lesions%20of%20cutaneous%20T-cell%20lymphoma%20resemble%20EPF.%22%2C%22date%22%3A%222013-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2F1346-8138.12125%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221346-8138%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A57%3A35Z%22%7D%7D%2C%7B%22key%22%3A%2277CIHPQY%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Nomura%20et%20al.%22%2C%22parsedDate%22%3A%222016-08%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BNomura%20T%2C%20Katoh%20M%2C%20Yamamoto%20Y%2C%20Miyachi%20Y%2C%20Kabashima%20K.%20Eosinophilic%20pustular%20folliculitis%3A%20A%20published%20work-based%20comprehensive%20analysis%20of%20therapeutic%20responsiveness.%20J%20Dermatol.%202016%20Aug%3B43%288%29%3A919%26%23x2013%3B27.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20pustular%20folliculitis%3A%20A%20published%20work-based%20comprehensive%20analysis%20of%20therapeutic%20responsiveness%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Takashi%22%2C%22lastName%22%3A%22Nomura%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mayumi%22%2C%22lastName%22%3A%22Katoh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yosuke%22%2C%22lastName%22%3A%22Yamamoto%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yoshiki%22%2C%22lastName%22%3A%22Miyachi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kenji%22%2C%22lastName%22%3A%22Kabashima%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20is%20a%20non-infectious%20inflammatory%20dermatosis%20of%20unknown%20etiology%20that%20principally%20affects%20the%20hair%20follicles.%20There%20are%20three%20variants%20of%20EPF%3A%20%28i%29%20classic%20EPF%3B%20%28ii%29%20immunosuppression-associated%20EPF%2C%20which%20is%20subdivided%20into%20HIV-associated%20%28IS%5C%2FHIV%29%20and%20non-HIV-associated%20%28IS%5C%2Fnon-HIV%29%3B%20and%20%28iii%29%20infancy-associated%20EPF.%20Oral%20indomethacin%20is%20efficacious%2C%20especially%20for%20classic%20EPF.%20No%20comprehensive%20information%20on%20the%20efficacies%20of%20other%20medical%20management%20regimens%20is%20currently%20available.%20In%20this%20study%2C%20we%20surveyed%20regimens%20for%20EPF%20that%20were%20described%20in%20articles%20published%20between%201965%20and%202013.%20In%20total%2C%20there%20were%201171%20regimens%3B%20874%2C%20137%2C%2045%20and%20115%20of%20which%20were%20applied%20to%20classic%2C%20IS%5C%2FHIV%2C%20IS%5C%2Fnon-HIV%20and%20infancy-associated%20EPF%2C%20respectively.%20Classic%20EPF%20was%20preferentially%20treated%20with%20oral%20indomethacin%20with%20efficacy%20of%2084%25%20whereas%20topical%20steroids%20were%20preferred%20for%20IS%5C%2FHIV%2C%20IS%5C%2Fnon-HIV%20and%20infancy-associated%20EPF%20with%20efficacy%20of%2047%25%2C%2073%25%20and%2082%25%2C%20respectively.%20Other%20regimens%20such%20as%20oral%20Sairei-to%20%28a%20Chinese-Japanese%20herbal%20medicine%29%2C%20diaminodiphenyl%20sulfone%2C%20cyclosporin%20and%20topical%20tacrolimus%20were%20effective%20for%20indomethacin-resistant%20cases.%20Although%20the%20preclusion%20of%20direct%20comparison%20among%20cases%20was%20one%20limitation%2C%20this%20study%20provides%20a%20dataset%20that%20is%20applicable%20to%20the%20construction%20of%20therapeutic%20algorithms%20for%20EPF.%22%2C%22date%22%3A%222016-08%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2F1346-8138.13287%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221346-8138%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A56%3A33Z%22%7D%7D%2C%7B%22key%22%3A%223JCALIA6%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Nomura%20et%20al.%22%2C%22parsedDate%22%3A%222016-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BNomura%20T%2C%20Katoh%20M%2C%20Yamamoto%20Y%2C%20Miyachi%20Y%2C%20Kabashima%20K.%20Eosinophilic%20pustular%20folliculitis%3A%20A%20proposal%20of%20diagnostic%20and%20therapeutic%20algorithms.%20J%20Dermatol.%202016%20Nov%3B43%2811%29%3A1301%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20pustular%20folliculitis%3A%20A%20proposal%20of%20diagnostic%20and%20therapeutic%20algorithms%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Takashi%22%2C%22lastName%22%3A%22Nomura%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mayumi%22%2C%22lastName%22%3A%22Katoh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yosuke%22%2C%22lastName%22%3A%22Yamamoto%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yoshiki%22%2C%22lastName%22%3A%22Miyachi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Kenji%22%2C%22lastName%22%3A%22Kabashima%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20is%20a%20sterile%20inflammatory%20dermatosis%20of%20unknown%20etiology.%20In%20addition%20to%20classic%20EPF%2C%20which%20affects%20otherwise%20healthy%20individuals%2C%20an%20immunocompromised%20state%20can%20cause%20immunosuppression-associated%20EPF%20%28IS-EPF%29%2C%20which%20may%20be%20referred%20to%20dermatologists%20in%20inpatient%20services%20for%20assessments.%20Infancy-associated%20EPF%20%28I-EPF%29%20is%20the%20least%20characterized%20subtype%2C%20being%20observed%20mainly%20in%20non-Japanese%20infants.%20Diagnosis%20of%20EPF%20is%20challenging%20because%20its%20lesions%20mimic%20those%20of%20other%20common%20diseases%2C%20such%20as%20acne%20and%20dermatomycosis.%20Furthermore%2C%20there%20is%20no%20consensus%20regarding%20the%20treatment%20for%20each%20subtype%20of%20EPF.%20Here%2C%20we%20created%20procedure%20algorithms%20that%20facilitate%20the%20diagnosis%20and%20selection%20of%20therapeutic%20options%20on%20the%20basis%20of%20published%20work%20available%20in%20the%20public%20domain.%20Our%20diagnostic%20algorithm%20comprised%20a%20simple%20flowchart%20to%20direct%20physicians%20toward%20proper%20diagnosis.%20Recommended%20regimens%20were%20summarized%20in%20an%20easy-to-comprehend%20therapeutic%20algorithm%20for%20each%20subtype%20of%20EPF.%20These%20algorithms%20would%20facilitate%20the%20diagnostic%20and%20therapeutic%20procedure%20of%20EPF.%22%2C%22date%22%3A%222016-11%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2F1346-8138.13359%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221346-8138%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A57%3A21Z%22%7D%7D%2C%7B%22key%22%3A%22QKB85JB8%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Marasca%20et%20al.%22%2C%22parsedDate%22%3A%222020%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BMarasca%20C%2C%20Ruggiero%20A%2C%20Fabbrocini%20G%2C%20Megna%20M.%20A%20Case%20of%20Ofuji%20Disease%20Successfully%20Treated%20with%20the%20Combination%20of%20Low-Dose%20Indomethacin%20and%20Topical%20Tacrolimus.%20Case%20Rep%20Dermatol.%202020%3B12%282%29%3A155%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20Case%20of%20Ofuji%20Disease%20Successfully%20Treated%20with%20the%20Combination%20of%20Low-Dose%20Indomethacin%20and%20Topical%20Tacrolimus%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Claudio%22%2C%22lastName%22%3A%22Marasca%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Angelo%22%2C%22lastName%22%3A%22Ruggiero%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gabriella%22%2C%22lastName%22%3A%22Fabbrocini%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Matteo%22%2C%22lastName%22%3A%22Megna%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20%28Ofuji%20disease%29%20is%20a%20chronic%2C%20noninfectious%20pruritic%20cutaneous%20disorder%20of%20unknown%20etiology.%20No%20official%20guidelines%20are%20available%20for%20its%20treatment.%20Herein%20we%20present%20the%20case%20of%20a%2059-year-old%20Caucasian%20man%20admitted%20to%20our%20outpatient%20clinic%20due%20to%20a%20generalized%20itchy%20skin%20rash%20characterized%20by%20papulo-pustules%20involving%20the%20face%2C%20trunk%2C%20and%20limbs.%20Histological%20examination%20supported%20the%20clinical%20diagnosis%20of%20EPF%20%28Ofuji%20disease%29.%20The%20combination%20of%20low-dose%20oral%20indomethacin%20and%20topical%20tacrolimus%20ointment%20once%20a%20day%20led%20to%20a%20complete%20resolution%20of%20the%20lesions%20as%20well%20as%20associated%20symptoms%20in%208%20weeks.%22%2C%22date%22%3A%222020%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1159%5C%2F000509176%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221662-6567%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A55%3A37Z%22%7D%7D%2C%7B%22key%22%3A%22BD4ULV3R%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Fertitta%20et%20al.%22%2C%22parsedDate%22%3A%222022-06-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFertitta%20L%2C%20Bodemer%20C%2C%20Molina%20T%2C%20Frassati-Biaggi%20A%2C%20Fraitag%20S%2C%20Leclerc-Mercier%20S.%20Eosinophilic%20Pustular%20Folliculitis%20of%20Infancy%3A%20A%20Histologic%20Assessment%20of%2043%20Cases.%20Am%20J%20Dermatopathol.%202022%20June%201%3B44%286%29%3A395%26%23x2013%3B403.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20Pustular%20Folliculitis%20of%20Infancy%3A%20A%20Histologic%20Assessment%20of%2043%20Cases%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Laura%22%2C%22lastName%22%3A%22Fertitta%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christine%22%2C%22lastName%22%3A%22Bodemer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thierry%22%2C%22lastName%22%3A%22Molina%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Annonciade%22%2C%22lastName%22%3A%22Frassati-Biaggi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sylvie%22%2C%22lastName%22%3A%22Fraitag%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22St%5Cu00e9phanie%22%2C%22lastName%22%3A%22Leclerc-Mercier%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20of%20infancy%20is%20a%20sterile%2C%20inflammatory%20dermatosis%20that%20mainly%20affects%20children%20younger%20than%2036%20months.%20The%20underlying%20physiopathologic%20mechanism%20is%20unclear.%20Clinical%20diagnosis%20is%20challenging%2C%20and%20a%20skin%20biopsy%20may%20be%20necessary.%20The%20literature%20data%20are%20sometimes%20contradictory%2C%20and%20a%20histologic%20series%20of%20eosinophilic%20pustular%20folliculitis%20of%20infancy%20cases%20has%20not%20been%20previously%20published.%22%2C%22date%22%3A%222022-06-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1097%5C%2FDAD.0000000000002006%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221533-0311%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A53%3A16Z%22%7D%7D%2C%7B%22key%22%3A%22629IMP68%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Gallo%20et%20al.%22%2C%22parsedDate%22%3A%222022-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BGallo%20G%2C%20Conti%20L%2C%20Quaglino%20P%2C%20Ribero%20S.%20Treatment%20of%20eosinophilic%20pustular%20folliculitis%20with%20low-dose%20isotretinoin.%20Int%20J%20Dermatol.%202022%20July%3B61%287%29%3Ae262%26%23x2013%3B4.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Treatment%20of%20eosinophilic%20pustular%20folliculitis%20with%20low-dose%20isotretinoin%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Giuseppe%22%2C%22lastName%22%3A%22Gallo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Luca%22%2C%22lastName%22%3A%22Conti%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Pietro%22%2C%22lastName%22%3A%22Quaglino%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Simone%22%2C%22lastName%22%3A%22Ribero%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222022-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fijd.15929%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221365-4632%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A55%3A25Z%22%7D%7D%2C%7B%22key%22%3A%22R4UM39IK%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Li%20et%20al.%22%2C%22parsedDate%22%3A%222023%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLi%20Y%2C%20Chen%20G%2C%20Zhou%20X%2C%20Zheng%20X%2C%20Zhang%20M%2C%20Yao%20X%2C%20et%20al.%20Clinical%20and%20Pathological%20Analysis%20of%2010%20Cases%20of%20Eosinophilic%20Pustular%20Folliculitis.%20Clin%20Cosmet%20Investig%20Dermatol.%202023%3B16%3A2467%26%23x2013%3B72.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Clinical%20and%20Pathological%20Analysis%20of%2010%20Cases%20of%20Eosinophilic%20Pustular%20Folliculitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yuan%22%2C%22lastName%22%3A%22Li%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gaihe%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xin%22%2C%22lastName%22%3A%22Zhou%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xiaole%22%2C%22lastName%22%3A%22Zheng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ming%22%2C%22lastName%22%3A%22Zhang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xiaojuan%22%2C%22lastName%22%3A%22Yao%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jiejie%22%2C%22lastName%22%3A%22Lu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xiaohuan%22%2C%22lastName%22%3A%22Hu%22%7D%5D%2C%22abstractNote%22%3A%22We%20conducted%20a%20retrospective%20analysis%20of%20clinical%20and%20pathologic%20data%20from%20January%202020%20to%20June%202023%2C%20focusing%20on%2010%20patients%20diagnosed%20with%20eosinophilic%20pustular%20folliculitis%20at%20our%20dermatology%20clinic.%20Four%20of%20the%20ten%20patients%20had%20the%20first%20rash%20on%20the%20face%2C%20five%20on%20the%20trunk%2C%20and%20one%20on%20the%20palms%20and%20feet%2C%20all%20of%20which%20were%20initially%20scattered%20papules%20that%20gradually%20increased%20and%20fused%20into%20erythematous%20plaques%20with%20a%20circular%20distribution.%20Seven%20had%20pustules%20with%20small%20surface%20desquamation%2C%20and%20three%20cases%20had%20micro%20swelling%20on%20the%20face.%20The%20rash%20involved%20only%20the%20face%20in%205%20cases%2C%20the%20face%20and%20trunk%20in%205%20cases%2C%20and%20the%20face%2C%20trunk%2C%20hands%2C%20and%20feet%20in%201%20case.%20Seven%20of%20the%20ten%20patients%20were%20pruritic%2C%20and%203%20had%20no%20obvious%20pruritus.%20The%20histopathological%20features%20were%20mild%20epidermal%20hyperplasia%2C%20lymphocytic%20and%20eosinophilic%20infiltration%20around%20the%20superficial%20middle%20dermal%20vessels%20and%20appendages%2C%20and%20eosinophilic%20and%20neutrophilic%20abscesses%20in%20the%20local%20hair%20follicles.%20Treatment%20with%20oral%20indomethacin%2C%20prednisone%2C%20and%20minocycline%20was%20effective.%22%2C%22date%22%3A%222023%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.2147%5C%2FCCID.S427718%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221178-7015%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A57%3A05Z%22%7D%7D%2C%7B%22key%22%3A%22ULEUQ44U%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Chen%20et%20al.%22%2C%22parsedDate%22%3A%222023-04-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BChen%20J%2C%20Beatty%20CJ%2C%20Falcone%20LM%2C%20English%20JC%2C%20Kazlouskaya%20V.%20Eosinophilic%20Pustular%20Folliculitis%20in%20the%20Setting%20of%20Solid%20Organ%20Transplant%20Immunosuppression.%20Dermatol%20Pract%20Concept.%202023%20Apr%201%3B13%282%29%3Ae2023078.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eosinophilic%20Pustular%20Folliculitis%20in%20the%20Setting%20of%20Solid%20Organ%20Transplant%20Immunosuppression%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeffrey%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Colleen%20J.%22%2C%22lastName%22%3A%22Beatty%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lauryn%20M.%22%2C%22lastName%22%3A%22Falcone%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Joseph%20C.%22%2C%22lastName%22%3A%22English%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Viktoryia%22%2C%22lastName%22%3A%22Kazlouskaya%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222023-04-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.5826%5C%2Fdpc.1302a78%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222160-9381%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A53%3A47Z%22%7D%7D%2C%7B%22key%22%3A%22BZJAB3VV%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ottavi%20et%20al.%22%2C%22parsedDate%22%3A%222024-01-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BOttavi%20M%2C%20Velin%20M%2C%20Cardot%20Leccia%20N%2C%20Passeron%20T.%20Successful%20Treatment%20of%20Eosinophilic%20Pustular%20Folliculitis%20With%20Dupilumab.%20JAMA%20Dermatol.%202024%20Jan%201%3B160%281%29%3A114%26%23x2013%3B5.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Successful%20Treatment%20of%20Eosinophilic%20Pustular%20Folliculitis%20With%20Dupilumab%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marie%22%2C%22lastName%22%3A%22Ottavi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marine%22%2C%22lastName%22%3A%22Velin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nathalie%22%2C%22lastName%22%3A%22Cardot%20Leccia%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Thierry%22%2C%22lastName%22%3A%22Passeron%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222024-01-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1001%5C%2Fjamadermatol.2023.4305%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222168-6084%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A55%3A12Z%22%7D%7D%2C%7B%22key%22%3A%22IFPEYTSL%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Chersi%20et%20al.%22%2C%22parsedDate%22%3A%222024-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BChersi%20F%2C%20Zelin%20E%2C%20Mazzoletti%20V%2C%20Caro%20Caposiena%20DR%2C%20Hasa%20Z%2C%20Nan%20K%2C%20et%20al.%20Mepolizumab%20therapy%20for%20eosinophilic%20pustular%20folliculitis%20%28Ofuji%20disease%29.%20J%20Eur%20Acad%20Dermatol%20Venereol.%202024%20Nov%3B38%2811%29%3Ae993%26%23x2013%3B6.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Mepolizumab%20therapy%20for%20eosinophilic%20pustular%20folliculitis%20%28Ofuji%20disease%29%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Filippo%22%2C%22lastName%22%3A%22Chersi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Enrico%22%2C%22lastName%22%3A%22Zelin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vanessa%22%2C%22lastName%22%3A%22Mazzoletti%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Dante%20Raffaele%22%2C%22lastName%22%3A%22Caro%20Caposiena%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zyber%22%2C%22lastName%22%3A%22Hasa%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Katiuscia%22%2C%22lastName%22%3A%22Nan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Diego%22%2C%22lastName%22%3A%22Signoretto%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Iris%22%2C%22lastName%22%3A%22Zalaudek%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nicola%22%2C%22lastName%22%3A%22di%20Meo%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222024-11%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fjdv.20047%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221468-3083%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A54%3A48Z%22%7D%7D%2C%7B%22key%22%3A%227HW9IZ2J%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Cai%20et%20al.%22%2C%22parsedDate%22%3A%222024-12%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BCai%20L%2C%20Yan%20Y%2C%20Li%20Y%2C%20Lin%20J%2C%20She%20X%2C%20Wang%20X.%20Two%20cases%20of%20eosinophilic%20pustular%20folliculitis%20successfully%20treated%20with%20abrocitinib.%20J%20Dermatol.%202024%20Dec%3B51%2812%29%3A1694%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Two%20cases%20of%20eosinophilic%20pustular%20folliculitis%20successfully%20treated%20with%20abrocitinib%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Liting%22%2C%22lastName%22%3A%22Cai%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yunling%22%2C%22lastName%22%3A%22Yan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yang%22%2C%22lastName%22%3A%22Li%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Junjie%22%2C%22lastName%22%3A%22Lin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xinyan%22%2C%22lastName%22%3A%22She%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xiaohua%22%2C%22lastName%22%3A%22Wang%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20is%20a%20rare%2C%20non-infectious%2C%20inflammatory%20disease%20characterized%20by%20an%20eosinophil-dominated%20infiltrate%20within%20and%20around%20pilosebaceous%20units.%20Sometimes%2C%20EPF%20manifests%20with%20eruptions%20in%20follicle-free%20areas%2C%20although%20it%20is%20not%20common%2C%20and%20treatment%20may%20be%20difficult.%20In%20this%20case%20study%20we%20report%20two%20patients%20with%20refractory%20EPF%20who%20presented%20with%20eruptions%20of%20both%20classic%20follicle%20areas%20and%20follicle-free%20areas.%20These%20two%20patients%20were%20successfully%20treated%20with%20abrocitinib%20after%20treatment%20failure%20with%20several%20traditional%20therapies%2C%20such%20as%20indomethacin%2C%20steroids%2C%20and%20cyclosporin.%20One%20patient%20achieved%20complete%20remission%20at%20week%204%20and%20the%20other%20at%20week%201%2C%20with%20no%20reported%20adverse%20effects.%20Therefore%2C%20we%20believe%20that%20abrocitinib%20may%20be%20a%20viable%20and%20safe%20therapeutic%20option%20for%20refractory%20EPF.%22%2C%22date%22%3A%222024-12%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2F1346-8138.17284%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221346-8138%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A54%3A31Z%22%7D%7D%2C%7B%22key%22%3A%22NFG7JJ3E%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Zheng%20et%20al.%22%2C%22parsedDate%22%3A%222024-12%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BZheng%20C%2C%20Yu%20Y%2C%20Zhou%20G%2C%20Liu%20H.%20A%20case%20of%20generalized%20eosinophilic%20pustular%20folliculitis%3A%20treatment%20with%20JAK%20inhibitor.%20J%20Dermatolog%20Treat.%202024%20Dec%3B35%281%29%3A2331785.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22A%20case%20of%20generalized%20eosinophilic%20pustular%20folliculitis%3A%20treatment%20with%20JAK%20inhibitor%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Chunzhi%22%2C%22lastName%22%3A%22Zheng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yueqian%22%2C%22lastName%22%3A%22Yu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Guizhi%22%2C%22lastName%22%3A%22Zhou%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hong%22%2C%22lastName%22%3A%22Liu%22%7D%5D%2C%22abstractNote%22%3A%22AIM%3A%20This%20case%20study%20aims%20to%20report%20the%20efficacy%20and%20safety%20of%20a%20Janus%20kinase%20%28JAK%29%20inhibitor%20in%20the%20treatment%20of%20generalized%20eosinophilic%20pustular%20folliculitis%20%28EPF%29.%5CnMETHODS%3A%20We%20present%20a%20case%20of%20a%2016-year-old%20Chinese%20patient%20who%20had%20been%20suffering%20from%20EPF%20for%20two%20years%20and%20had%20shown%20no%20response%20to%20both%20topical%20and%20systemic%20glucocorticoids.%20The%20patient%20was%20subsequently%20treated%20with%20oral%20tofacitinib%20at%20a%20dosage%20of%205mg%20daily.%5CnRESULTS%3A%20Significant%20remission%20of%20eruption%20and%20pruritus%20was%20observed%20in%20the%20patient%20upon%20treatment%20with%20tofacitinib.%20However%2C%20a%20relapse%20occurred%20upon%20dose%20reduction.%20Subsequent%20switch%20to%20the%20highly%20selective%20JAK1%20inhibitor%20upadacitinib%20resulted%20in%20complete%20recovery%2C%20with%20the%20patient%20achieving%20a%20symptom-free%20status%20after%20six%20months.%5CnCONCLUSIONS%3A%20JAK%20inhibitors%20show%20promise%20as%20a%20potential%20treatment%20option%20for%20EPF%20patients%20who%20do%20not%20respond%20to%20traditional%20therapies.%22%2C%22date%22%3A%222024-12%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1080%5C%2F09546634.2024.2331785%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221471-1753%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A55%3A01Z%22%7D%7D%2C%7B%22key%22%3A%222PZCLNCK%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Dodia%20and%20Cook%22%2C%22parsedDate%22%3A%222025%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDodia%20P%2C%20Cook%20C.%20Eosinophilic%20Pustular%20Folliculitis.%20In%3A%20StatPearls.%20Treasure%20Island%20%28FL%29%3A%20StatPearls%20Publishing%3B%202025.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22bookSection%22%2C%22title%22%3A%22Eosinophilic%20Pustular%20Folliculitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Paarth%22%2C%22lastName%22%3A%22Dodia%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Christopher%22%2C%22lastName%22%3A%22Cook%22%7D%5D%2C%22abstractNote%22%3A%22Eosinophilic%20pustular%20folliculitis%20%28EPF%29%2C%20first%20reported%20in%201965%20and%20previously%20known%20as%20Ofuji%20disease%2C%20is%20a%20rare%20dermatological%20condition%20found%20across%20diverse%20patient%20populations.%20EPF%20comprises%20three%20distinct%20subtypes%3A%20EPF%20of%20infancy%20%28EPFI%29%2C%20classic%20EPF%20of%20adulthood%20%28EPF%29%2C%20and%20immunosuppression-associated%20EPF%20%28IS-EPF%29.%20All%20three%20subtypes%20are%20characterized%20by%20a%20pruritic%20pustular%20skin%20eruption%20with%20a%20noninfectious%20origin%20and%20histological%20eosinophilic%20infiltrates.%20However%2C%20despite%20these%20similarities%2C%20treatment%20approaches%20and%20prognoses%20vary%20with%20each%20subtype.%20This%20activity%20will%20review%20the%20epidemiology%2C%20proposed%20etiologies%2C%20presumptive%20pathophysiological%20processes%2C%20typical%20clinical%20presentation%2C%20evaluation%2C%20and%20management%20of%20EPF%20and%20highlight%20the%20role%20of%20the%20interprofessional%20team%20in%20caring%20for%20patients%20with%20this%20dermatological%20condition.%22%2C%22bookTitle%22%3A%22StatPearls%22%2C%22date%22%3A%222025%22%2C%22originalDate%22%3A%22%22%2C%22originalPublisher%22%3A%22%22%2C%22originalPlace%22%3A%22%22%2C%22format%22%3A%22%22%2C%22ISBN%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22ISSN%22%3A%22%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-09T16%3A25%3A49Z%22%7D%7D%2C%7B%22key%22%3A%22PLVX28NU%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Wang%20et%20al.%22%2C%22parsedDate%22%3A%222025-02-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWang%20QX%2C%20He%20HY%2C%20Niu%20YL%2C%20Fang%20S.%20Refractory%20eosinophilic%20pustular%20folliculitis%20treated%20with%20tofacitinib%3A%20a%20case%20series%20and%20literature%20review.%20Clin%20Exp%20Dermatol.%202025%20Feb%201%3Bllaf053.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Refractory%20eosinophilic%20pustular%20folliculitis%20treated%20with%20tofacitinib%3A%20a%20case%20series%20and%20literature%20review%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Qin-Xiao%22%2C%22lastName%22%3A%22Wang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hai-Yang%22%2C%22lastName%22%3A%22He%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ying-Luo%22%2C%22lastName%22%3A%22Niu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sheng%22%2C%22lastName%22%3A%22Fang%22%7D%5D%2C%22abstractNote%22%3A%22OBJECTIVES%3A%20Eosinophilic%20pustular%20folliculitis%20%28EPF%29%20is%20an%20uncommon%20skin%20condition%20that%20presents%20as%20follicular%20papules%20or%20pustules.%20The%20treatment%20of%20EPF%20is%20challenging%20due%20to%20the%20high%20relapse%20rates.%20This%20study%20aimed%20to%20evaluate%20the%20efficacy%20and%20safety%20of%20tofacitinib%20as%20a%20treatment%20for%20EPF.%5CnMETHODS%3A%20We%20presented%203%20patients%20with%20refractory%20EPF%20who%20had%20been%20successfully%20treated%20with%20tofacitinib%20at%20our%20clinic%20and%20conducted%20a%20literature%20review%20using%20the%20PubMed%20database%20to%20gain%20further%20insight%20into%20this%20promising%20therapy.%5CnRESULTS%3A%20Our%20patients%20were%20effectively%20treated%20with%20tofacitinib.%20To%20date%2C%20only%20three%20patients%20with%20EPF%20treated%20with%20Janus%20kinase%20%28JAK%29%20inhibitors%20have%20been%20reported%20and%20reviewed%3A%20one%20treated%20with%20tofacitinib%20and%20two%20with%20abrocitinib.%20Complete%20remission%20was%20observed%20in%20all%20the%20above%20patients%2C%20with%20no%20adverse%20events%20or%20relapses%20reported%20during%20an%20average%20follow-up%20period%20of%204.3%20months.%5CnCONCLUSION%3A%20Tofacitinib%20may%20be%20an%20emerging%20alternative%20treatment%20option%20for%20EFP%20patients.%20Larger%20randomized%20controlled%20studies%20are%20needed%20to%20confirm%20these%20findings.%22%2C%22date%22%3A%222025-02-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1093%5C%2Fced%5C%2Fllaf053%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221365-2230%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A54%3A03Z%22%7D%7D%2C%7B%22key%22%3A%22B7IUMP5G%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Tan%20et%20al.%22%2C%22parsedDate%22%3A%222025-03-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BTan%20X%2C%20Nie%20S%2C%20Chen%20B%2C%20Wu%20Z.%20Successful%20Treatment%20of%20Eosinophilic%20Pustular%20Folliculitis%20With%20Dupilumab%20in%20a%209-Year-Old%20Boy.%20Pediatr%20Dermatol.%202025%20Mar%206%3B%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Successful%20Treatment%20of%20Eosinophilic%20Pustular%20Folliculitis%20With%20Dupilumab%20in%20a%209-Year-Old%20Boy%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Xi%22%2C%22lastName%22%3A%22Tan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Shu%22%2C%22lastName%22%3A%22Nie%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bin%22%2C%22lastName%22%3A%22Chen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Zhouwei%22%2C%22lastName%22%3A%22Wu%22%7D%5D%2C%22abstractNote%22%3A%22A%209-year-old%20boy%20with%20eosinophilic%20pustular%20folliculitis%20%28EPF%29%20was%20successfully%20treated%20with%20dupilumab.%20While%20reported%20in%20adult%20EPF%2C%20this%20is%20the%20first%20case%20of%20EPF%20treated%20with%20dupilumab%20in%20a%20child.%20Our%20case%20suggests%20dupilumab%20might%20be%20a%20favorable%20therapeutic%20option%20for%20EPF%20in%20children.%20Further%20research%20is%20needed%20to%20fully%20elucidate%20the%20efficacy%20and%20safety%20of%20dupilumab%20in%20children%20with%20EPF%20and%20to%20identify%20predictive%20factors%20for%20treatment%20response.%22%2C%22date%22%3A%222025-03-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fpde.15908%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221525-1470%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%226WBZAKM9%22%5D%2C%22dateModified%22%3A%222025-05-01T15%3A54%3A17Z%22%7D%7D%5D%7D 1.
Ofuji S, Ogino A, Horio T, Oseko T, Uehara M. Eosinophilic pustular folliculitis. Acta Derm Venereol. 1970;50(3):195–203.
1.
Ishibashi A, Nishiyama Y, Miyata C, Chujo T. Eosinophilic pustular folliculitis (ofuji). Dermatologica. 1974;149(4):240–7.
1.
Nervi SJ, Schwartz RA, Dmochowski M. Eosinophilic pustular folliculitis: a 40 year retrospect. J Am Acad Dermatol. 2006 Aug;55(2):285–9.
1.
Sufyan W, Tan KB, Wong ST, Lee YS. Eosinophilic pustular folliculitis. Arch Pathol Lab Med. 2007 Oct;131(10):1598–601.
1.
Fujiyama T, Tokura Y. Clinical and histopathological differential diagnosis of eosinophilic pustular folliculitis. J Dermatol. 2013 June;40(6):419–23.
1.
Nomura T, Katoh M, Yamamoto Y, Miyachi Y, Kabashima K. Eosinophilic pustular folliculitis: A published work-based comprehensive analysis of therapeutic responsiveness. J Dermatol. 2016 Aug;43(8):919–27.
1.
Nomura T, Katoh M, Yamamoto Y, Miyachi Y, Kabashima K. Eosinophilic pustular folliculitis: A proposal of diagnostic and therapeutic algorithms. J Dermatol. 2016 Nov;43(11):1301–6.
1.
Marasca C, Ruggiero A, Fabbrocini G, Megna M. A Case of Ofuji Disease Successfully Treated with the Combination of Low-Dose Indomethacin and Topical Tacrolimus. Case Rep Dermatol. 2020;12(2):155–8.
1.
Fertitta L, Bodemer C, Molina T, Frassati-Biaggi A, Fraitag S, Leclerc-Mercier S. Eosinophilic Pustular Folliculitis of Infancy: A Histologic Assessment of 43 Cases. Am J Dermatopathol. 2022 June 1;44(6):395–403.
1.
Gallo G, Conti L, Quaglino P, Ribero S. Treatment of eosinophilic pustular folliculitis with low-dose isotretinoin. Int J Dermatol. 2022 July;61(7):e262–4.
1.
Li Y, Chen G, Zhou X, Zheng X, Zhang M, Yao X, et al. Clinical and Pathological Analysis of 10 Cases of Eosinophilic Pustular Folliculitis. Clin Cosmet Investig Dermatol. 2023;16:2467–72.
1.
Chen J, Beatty CJ, Falcone LM, English JC, Kazlouskaya V. Eosinophilic Pustular Folliculitis in the Setting of Solid Organ Transplant Immunosuppression. Dermatol Pract Concept. 2023 Apr 1;13(2):e2023078.
1.
Ottavi M, Velin M, Cardot Leccia N, Passeron T. Successful Treatment of Eosinophilic Pustular Folliculitis With Dupilumab. JAMA Dermatol. 2024 Jan 1;160(1):114–5.
1.
Chersi F, Zelin E, Mazzoletti V, Caro Caposiena DR, Hasa Z, Nan K, et al. Mepolizumab therapy for eosinophilic pustular folliculitis (Ofuji disease). J Eur Acad Dermatol Venereol. 2024 Nov;38(11):e993–6.
1.
Cai L, Yan Y, Li Y, Lin J, She X, Wang X. Two cases of eosinophilic pustular folliculitis successfully treated with abrocitinib. J Dermatol. 2024 Dec;51(12):1694–7.
1.
Zheng C, Yu Y, Zhou G, Liu H. A case of generalized eosinophilic pustular folliculitis: treatment with JAK inhibitor. J Dermatolog Treat. 2024 Dec;35(1):2331785.
1.
Dodia P, Cook C. Eosinophilic Pustular Folliculitis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
1.
Wang QX, He HY, Niu YL, Fang S. Refractory eosinophilic pustular folliculitis treated with tofacitinib: a case series and literature review. Clin Exp Dermatol. 2025 Feb 1;llaf053.
1.
Tan X, Nie S, Chen B, Wu Z. Successful Treatment of Eosinophilic Pustular Folliculitis With Dupilumab in a 9-Year-Old Boy. Pediatr Dermatol. 2025 Mar 6;